Opioid-Induced Vomiting: Causes, Risks, and What to Do
When you take opioids for pain, opioid-induced vomiting, a side effect caused by how opioids affect the brain’s vomiting center and gut motility. It’s not just discomfort—it’s a sign your body is reacting to the drug’s impact on your nervous system. This isn’t rare. Up to 40% of people on long-term opioids experience nausea or vomiting, especially when starting treatment or increasing the dose. Even if you’ve been on opioids for months, your body can suddenly start rejecting them. It’s not weakness. It’s biology.
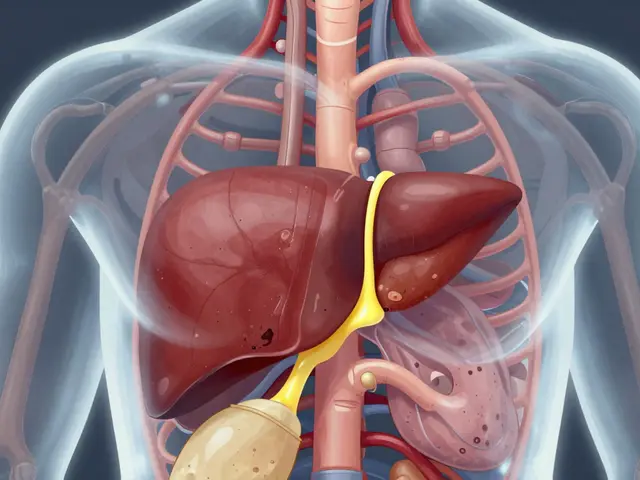
opioid side effects, a group of reactions including constipation, drowsiness, and vomiting, that stem from how these drugs bind to receptors in the brain and digestive tract don’t stop at nausea. The same receptors that dull pain also trigger the chemoreceptor trigger zone in your brainstem—your body’s vomiting alarm. And because opioids slow gut movement, food sits longer, making nausea worse. This isn’t just about feeling sick. Persistent vomiting can lead to dehydration, electrolyte imbalances, and even missed doses, which means your pain isn’t controlled. That’s a dangerous cycle.
Some people think switching opioids will fix it. Sometimes it does—morphine is more likely to cause vomiting than oxycodone or fentanyl. But the real fix often comes from antiemetic medications, drugs like ondansetron or metoclopramide that block the signals causing nausea and vomiting. These aren’t just band-aids. Used right, they let you stay on the pain relief you need without the misery. And if you’re on high doses or have kidney issues, your risk goes up. Older adults and those with a history of motion sickness or migraines are more likely to struggle with this side effect.
Don’t ignore it. If you’re vomiting after taking your opioid, talk to your provider. Don’t just stop the med—that can bring back severe pain. Don’t just push through—that can lead to hospital visits. There are proven ways to manage this. Some patients benefit from low-dose naltrexone, which can reduce nausea without blocking pain relief. Others find relief with ginger supplements or acupressure wristbands. What works varies, but the key is acting early.
What you’ll find in the posts below are real stories and science-backed strategies from people who’ve been there. From how to spot when vomiting signals a bigger problem, to what meds actually work without making you drowsy, to how to talk to your doctor without sounding like you’re complaining—this isn’t guesswork. It’s what works for real patients trying to stay on their treatment without losing their quality of life.

Chronic Opioid-Induced Nausea: Diet, Hydration, and Medication Options That Actually Work
Chronic opioid-induced nausea affects up to one-third of long-term users. Learn how diet, hydration, and medication choices-like opioid rotation and ginger-can reduce nausea without stopping pain relief.