Opioid Rotation Assistant
Current Opioid
Alternative Options
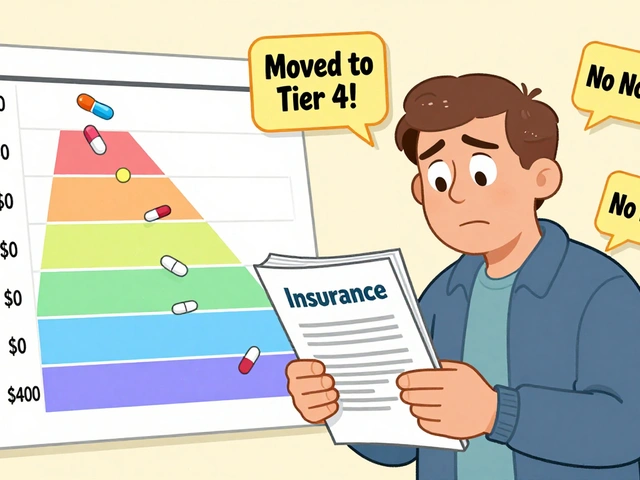
Oxycodone
Medium risk
Lower nausea risk than morphine
Conversion:
10mg morphine → 5-7.5mg oxycodone
Recommended antiemetics:
- Phenothiazines (prochlorperazine)
- Ondansetron (for breakthrough nausea)
Fentanyl Patch
Low risk
30-40% reduction in nausea for many patients
Conversion:
20mg morphine/day → 50-75mcg/hr patch
Recommended antiemetics:
- Dexamethasone
- Phenothiazines
Tapentadol
Low risk
Significantly lower nausea profile
Conversion:
10mg morphine → 50mg tapentadol
Recommended antiemetics:
- Ginger
- Phenothiazines
When you're taking opioids long-term for pain, nausea isn't just an annoyance-it can make you stop taking the medication altogether. About 1 in 3 people on chronic opioid therapy get stuck with persistent nausea that doesn't go away, even after the first week. This isn't normal side effects fading-it's chronic opioid-induced nausea, and it's more common than most doctors admit. For many, it's the second biggest reason to quit opioids, right after constipation. And if you're one of them, you're not broken. You're just dealing with a poorly understood side effect that hits different for everyone.
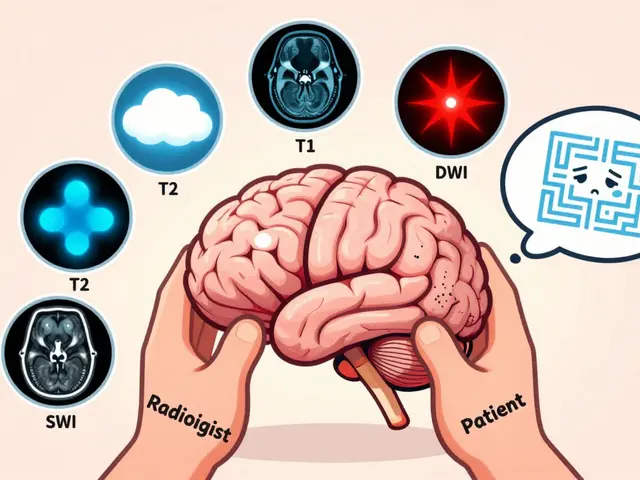
Why Your Body Keeps Feeling Sick
Opioids don't just block pain signals. They also mess with three key areas in your body that control nausea. First, they activate the chemoreceptor trigger zone in your brainstem-a little alarm system that gets fooled into thinking you've swallowed poison. Second, they slow down your gut, which triggers nausea through stretch receptors and delayed emptying. Third, and this one surprises most people, they interfere with your inner ear's balance system. That's why turning your head or standing up fast can make you feel like the room is spinning. It's not anxiety. It's your vestibular system being directly stimulated by the drug.Not all opioids are equal here. Oxymorphone? High risk. Oxycodone? Moderate. Tapentadol? Much lower. Even morphine and codeine vary wildly in how likely they are to make you nauseous, based on how tightly they bind to certain receptors. Your genetics play a role too-if you're a CYP2D6 poor metabolizer, codeine can turn into way more morphine than expected, making nausea worse. That’s why switching opioids isn't just about pain control-it's often the most effective way to reduce nausea.
Opioid Rotation: The Most Underused Tool
If you've been on the same opioid for months and still feel sick, it's time to consider a switch. This isn't a last resort-it's a standard tactic in palliative care. Studies show that rotating from morphine to oxycodone helps about half of patients with persistent nausea. Switching to a fentanyl patch can cut nausea by 30-40% for many, simply because it avoids the first-pass metabolism in the liver that creates more nausea-causing byproducts.But you can't just swap one pill for another. Methadone, for example, needs a 50-75% dose reduction when switching from other opioids because it builds up differently in your system. Do it wrong, and you risk overdose. Always work with a pain specialist or pharmacist who knows how to calculate these conversions. A 2021 survey of palliative care teams found that 78% of clinics have formal opioid rotation protocols-but only 42% of primary care practices do. Don't assume your regular doctor knows how to do this safely.
Medications That Actually Help (and Which to Avoid)
Not all antiemetics are created equal. Prochlorperazine and promethazine (phenothiazines) are the most commonly used and have the best real-world track record-65-70% of patients report improvement. They're cheap, too: a month's supply costs about $2-$5. Metoclopramide is the only prokinetic available in the U.S., meaning it speeds up your stomach emptying. It works for about 60% of people, but it can cause restlessness, tremors, or even parkinsonism with long-term use. The FDA warns against using it beyond 12 weeks.Ondansetron (Zofran) is expensive-around $35 per dose-but it's popular in hospitals and among patients who've tried everything else. Some studies suggest it's better for breakthrough nausea, especially if your nausea spikes after meals. But it's not a first-line fix for chronic cases. Dexamethasone helps some, but we don't fully understand why. And while haloperidol is sometimes used, it's less effective than phenothiazines and carries more sedation risk.
Here's what most patients don't know: antiemetics should be started from day one of opioid therapy. Eighty-two percent of palliative care providers co-prescribe them during the first 1-2 weeks. That’s because nausea often peaks early and can be prevented, not just treated after it hits. Waiting until you're vomiting every day means you're already behind.

Diet: What to Eat (and What to Skip)
Forget bland diets. The old advice to eat crackers and toast doesn't work for most people with chronic opioid nausea. A 2023 survey of 429 patients on PatientsLikeMe found that 63% felt better with protein-rich snacks-like Greek yogurt, hard-boiled eggs, or peanut butter on rice cakes-instead of carbs. Why? Protein helps stabilize blood sugar and slows gastric emptying in a way that reduces the sensation of nausea.Small, frequent meals are key. Instead of three big meals, aim for six to eight tiny ones-150 to 200 calories each. This keeps your stomach from getting too full or too empty, both of which trigger nausea. A 2022 University of Washington study showed 55% of patients improved with this approach. Avoid greasy, spicy, or overly sweet foods-they're harder to digest and worsen gut slowdown.
Ginger has real science behind it. In a 2021 analysis of pain forums, 78% of users who tried ginger chews (like Briess brand) reported moderate to significant relief. Ginger works by calming the gut and reducing inflammation in the digestive tract. Try 1-2 chews every 3-4 hours, or sip ginger tea made from fresh root. Don't rely on ginger capsules-they're less consistent in dose and absorption.
Hydration: Sip, Don't Chug
Drinking water is important, but chugging 8 glasses a day can make nausea worse. Large volumes stretch your stomach and slow gastric emptying even more. Instead, sip 2-4 ounces every 15-20 minutes. This keeps you hydrated without overwhelming your system.Electrolytes matter more than most realize. Opioids can cause mild dehydration through reduced fluid intake and increased sweating. Many patients find relief with oral rehydration solutions like Pedialyte or homemade versions (water + pinch of salt + teaspoon of honey). These help maintain sodium and potassium balance, which supports nerve and muscle function-including your gut.
Carbonated drinks? Avoid them. The bubbles increase stomach pressure and bloating. Cold fluids are often better tolerated than warm ones. Keep a small bottle of water or electrolyte drink by your bed and sip before getting up in the morning-many report their worst nausea hits at dawn.

Non-Medication Tactics That Work
Resting your head still reduces nausea by 35-40%, according to a 2017 study. Lying down with your head supported, eyes closed, and no sudden movements helps your brain stop getting conflicting signals from your inner ear and eyes. Don't just sit still-lie down. Even 20 minutes can reset your system.Acupressure bands (like Sea-Bands) worn on the inner wrist have mixed results, but many patients swear by them. They target the P6 point, which is linked to nausea control. It's low-risk, so it's worth trying.
And yes-your mental state matters. Fear of nausea can make it worse. When you're constantly worried about vomiting, your body goes into high alert, tightening muscles and increasing sensitivity. Cognitive behavioral techniques, even simple breathing exercises, can break that cycle. Try 4-7-8 breathing: inhale for 4 seconds, hold for 7, exhale for 8. Do it three times when nausea starts.
What’s on the Horizon
There's real hope coming. Researchers are testing low-dose naltrexone (0.5-1 mg daily), which blocks some opioid receptors in the brain without reducing pain relief. Early results show a 45% drop in nausea severity after 8 weeks. Janssen is developing a new drug that specifically blocks kappa-opioid receptors in the inner ear-the ones causing the dizziness and spinning sensation. If it works, it could be the first treatment that targets the root cause without touching pain control.Another promising area is gut microbiome research. Scientists at the University of Pittsburgh found that patients with certain gut bacteria had 32% higher rates of nausea resolution. Future treatments might include targeted probiotics or prebiotics tailored to opioid users.
For now, though, the best approach is still practical: rotate opioids if needed, use proven antiemetics early, eat small protein-rich meals, sip fluids slowly, rest your head, and avoid triggers. It’s not glamorous. But it works.
How long does opioid-induced nausea usually last?
For most people, nausea improves within 3 to 7 days as tolerance develops. But about 15-20% of patients continue to experience symptoms beyond two weeks-this is called chronic opioid-induced nausea. If it lasts longer than 14 days despite stable opioid dosing, it's not just a temporary side effect. It needs active management.
Can I just stop taking my opioid if I'm nauseous?
Stopping opioids suddenly can cause withdrawal, which includes its own set of nausea, sweating, and anxiety. That makes things worse. Instead of quitting, talk to your doctor about rotating to a different opioid or adding an antiemetic. The goal is to keep your pain controlled while reducing nausea-not to stop treatment entirely.
Is ginger really effective for opioid nausea?
Yes, in real-world use. Studies show ginger reduces nausea through multiple pathways: calming the stomach lining, reducing inflammation, and possibly blocking serotonin receptors in the gut. In patient surveys, 78% of those using ginger chews reported noticeable relief. It's not a cure, but it's one of the few non-drug options with consistent positive feedback. Stick with a trusted brand like Briess for reliable dosing.
Why does my nausea get worse in the morning?
Morning nausea is common because opioid levels in your blood often dip overnight, especially with short-acting drugs. This can trigger a rebound effect in the brain's nausea centers. Also, lying flat for hours can cause stomach acid to rise, and dehydration from overnight fluid loss adds to the problem. Sipping water or electrolytes before getting up, and eating a small protein snack right after waking, can help.
Are there any foods I should absolutely avoid?
Avoid fried, greasy, or spicy foods-they're harder to digest and worsen gut slowdown. Also skip large meals, sugary snacks, and carbonated drinks. Even strong smells (like coffee or cooking oil) can trigger nausea in sensitive individuals. Focus on bland, low-fat, protein-based snacks eaten slowly. If a food makes you feel worse, even once, write it down. Your personal triggers matter more than general advice.
When should I see a specialist for opioid nausea?
If you've tried basic strategies (diet, hydration, antiemetics) for more than 2 weeks with no improvement, or if your nausea is causing you to miss meals, lose weight, or feel dizzy when standing, it's time to see a pain or palliative care specialist. They know how to safely rotate opioids, adjust doses, and access newer treatments. Primary care doctors often lack the tools to manage chronic opioid side effects effectively.



Matthew Stanford
November 29, 2025 AT 18:32Been on oxycodone for 5 years. Switched to tapentadol last year and the nausea dropped off a cliff. No magic pill, just the right opioid for your body. Trust me, it’s worth the hassle of switching.
Also, ginger chews? Lifesaver. Briess brand only. Don’t waste your time with capsules.
Olivia Currie
December 1, 2025 AT 08:35OMG YES. I thought I was just weak for feeling sick all the time. I cried reading this. I’ve been hiding my nausea like it’s embarrassing. Turns out it’s not me-it’s the damn drugs. Thank you for naming it. I feel seen. 🥹
Curtis Ryan
December 1, 2025 AT 10:49so i tried the ginger thing and it kinda worked? not sure if it was the ginger or just me drinking water more often. but i swear i felt better. also pro tip: dont eat cereal in the morning. its a trap. protein rocks. eggs forever. 🤙
Rajiv Vyas
December 2, 2025 AT 07:09They don't want you to know this but the FDA and Big Pharma are hiding the real cause. Opioid nausea isn't from the drug-it's from the glyphosate in your food poisoning your gut. They profit off you taking more meds. Ginger? Nah. Detox with apple cider vinegar and lemon water. That's the real fix. #BigPharmaLies
farhiya jama
December 3, 2025 AT 15:45I read this whole thing. Then I cried. Then I went back to my couch and didn’t move for 3 hours. I’m too tired to try any of this. I just want the nausea to stop. But I don’t have the energy to switch meds or buy ginger chews. So… I guess I’ll keep vomiting.
Astro Service
December 4, 2025 AT 05:50Why are we letting foreigners tell us how to treat pain? In America we just tough it out. I don't need no ginger or yoga breathing. Take your pills like a man. And stop complaining about nausea. You're not a baby.
DENIS GOLD
December 4, 2025 AT 13:11So let me get this straight… you’re telling me the solution to opioid nausea is… eating protein? Sipping water? And not chugging? Wow. Groundbreaking. Next you’ll tell me breathing oxygen helps too. 🙄
Ifeoma Ezeokoli
December 4, 2025 AT 17:48As a nurse in Lagos, I’ve seen this over and over. People think it’s spiritual or punishment. But it’s biology. Your body is trying to tell you something. Listen. Try the rotation. Try ginger. Try the small meals. You’re not broken. You’re just fighting a system that doesn’t listen. I’m proud of you for seeking help.
❤️
Daniel Rod
December 5, 2025 AT 10:02This post made me think about how we treat pain like it’s a puzzle to solve, not a lived experience. We focus on the drugs, the doses, the nausea… but we forget the loneliness. The isolation. The way you start avoiding friends because you’re scared you’ll vomit at dinner.
Maybe the real cure isn’t in the pill or the ginger-it’s in being heard. Thank you for writing this. I needed it.
🫂
gina rodriguez
December 5, 2025 AT 11:39I love how practical this is. No fluff. Just real stuff that works. I shared this with my sister who’s on long-term morphine-she’s going to try the protein snacks and the sipping water trick. Small changes, big difference. You’re doing great work.
❤️
Sue Barnes
December 5, 2025 AT 13:59Ugh. Of course you’re still nauseous. You didn’t start the antiemetic on day one. That’s basic. You’re not following protocol. Stop making excuses. If you’d just listened to your doctor instead of Googling ginger, you wouldn’t be here.
jobin joshua
December 7, 2025 AT 03:08OMG I tried the sea-bands and it worked??? I thought they were placebo. But I wore them for 3 days and the spinning stopped. I’m not even kidding. 🤯🫶
Sachin Agnihotri
December 7, 2025 AT 07:05...I just want to say... that the CYP2D6 thing... it's real... my cousin... she's a poor metabolizer... and she went from codeine to oxymorphone... and it was like a nightmare... I'm just saying... genetic testing... it's not optional... it's essential... please... get tested... before you switch... please... please... please...
Diana Askew
December 8, 2025 AT 01:56Of course it's the government. They don't want you to know that the real cause is 5G radiation + fluoride in the water. Ginger? Please. You're being manipulated. Take naltrexone? No way. That's a mind-control drug. You think they'd let you fix nausea without controlling your soul? Wake up.