Over 900,000 people worldwide are diagnosed with liver cancer each year, and more than 8 in 10 of those cases happen in people who already have cirrhosis. That’s not a coincidence. Cirrhosis - scarring of the liver from long-term damage - is the single biggest risk factor for hepatocellular carcinoma (HCC), the most common type of primary liver cancer. The good news? When caught early, HCC is often treatable. The bad news? Most people don’t get screened, and by the time symptoms show up, it’s often too late.
Why Surveillance Matters More Than You Think
If you have cirrhosis, regular screening isn’t optional - it’s life-saving. Studies show that people who get checked every six months are up to 70% more likely to survive five years after diagnosis than those who don’t. Why? Because HCC grows fast. In a cirrhotic liver, tumors can go from invisible to the size of a golf ball in under six months. That’s why guidelines from the American Association for the Study of Liver Diseases (AASLD) and the European Association for the Study of the Liver (EASL) both say: every adult with cirrhosis should get an ultrasound every six months.Ultrasound is cheap, safe, and widely available. It doesn’t use radiation. It doesn’t require contrast dye. And it’s good enough to spot tumors bigger than 1 cm - the size at which curative treatments still work. But ultrasound alone isn’t perfect. That’s why some guidelines also suggest checking a blood marker called alpha-fetoprotein (AFP). If AFP is above 20 ng/mL, it’s a red flag. Not every elevated AFP means cancer - it can rise with inflammation or active hepatitis - but it’s a signal to dig deeper.
When an ultrasound shows something suspicious, the next step is always a contrast-enhanced CT or MRI scan. These scans show how blood flows through the liver, which helps doctors tell the difference between a harmless nodule and a tumor. The Liver Imaging Reporting and Data System (LI-RADS), updated in 2022, gives radiologists a standard way to describe what they see. A LI-RADS 5 result means the lesion is almost certainly HCC. That’s when treatment needs to start immediately.
Who Should Be Screened - And Who Doesn’t Need It
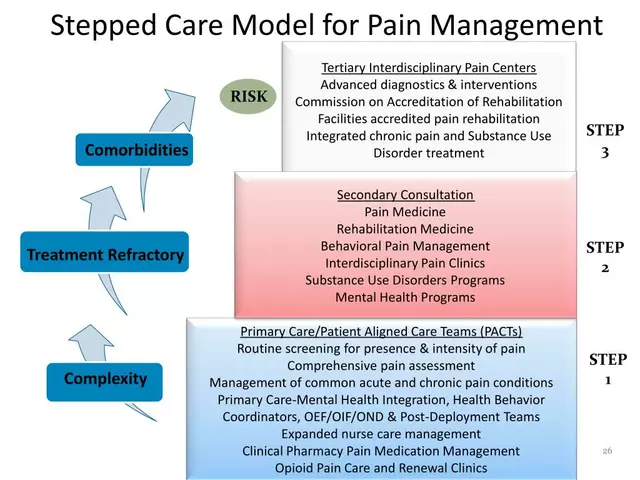
Not every person with cirrhosis is at the same risk. That’s where things get more nuanced. The old rule - screen everyone - is changing. New research shows that some people have such low risk that screening might do more harm than good, with unnecessary scans, anxiety, and costs.The EASL’s 2023 Policy Statement introduced a risk-based model. It divides cirrhotic patients into three groups:
- High-risk (over 2.5% annual risk): These are people with hepatitis B, active hepatitis C (even after cure), heavy alcohol use, or advanced scarring. They get ultrasound every six months - and some may soon get MRI instead.
- Medium-risk (1.5-2.5% annual risk): Includes most people with NAFLD (non-alcoholic fatty liver disease) after viral clearance or moderate alcohol use. They stick with standard ultrasound every six months.
- Low-risk (under 1.5% annual risk): People with stable, mild cirrhosis from causes like autoimmune hepatitis that’s well-controlled. They might not need routine screening, but should still be monitored by their doctor.
Meanwhile, the AASLD still recommends screening everyone with Child-Turcotte-Pugh (CTP) Class A or B cirrhosis - even if they’re older or have other health problems. But they explicitly say not to screen those with CTP Class C cirrhosis unless they’re on a transplant list. Why? Because their life expectancy is often less than two years, and HCC treatment won’t help much if the liver is failing.
There’s a big gap in the U.S. The U.S. Preventive Services Task Force hasn’t issued any official guidance. That leaves primary care doctors confused. In VA hospitals, only about 30-50% of eligible patients get screened. In community clinics? Sometimes less than 20%. That’s not because doctors don’t know - it’s because systems aren’t built to remind them.
How Treatment Depends on Stage and Liver Health
If HCC is found early - and only about 30% of cases are - there are real chances for cure. Treatment options depend on three things: tumor size and number, liver function, and whether the cancer has spread.Stage 0 or A (very early): Tumors are small (under 2 cm), single, and the liver still works well. Options include:
- Radiofrequency ablation (RFA): A needle is inserted through the skin, guided by ultrasound, and heated to burn the tumor. Success rates are over 85% for tumors under 2 cm.
- Microwave ablation: Similar to RFA but uses microwaves. Faster, works better near big blood vessels.
- Surgical resection: Removing the tumor. Only possible if the liver is healthy enough to regenerate. Usually reserved for younger patients with minimal scarring.
Stage B (intermediate): Multiple tumors, or one larger tumor, but no spread outside the liver. The go-to treatment is transarterial chemoembolization (TACE). A catheter is threaded into the liver artery, and chemo drugs plus tiny beads are delivered directly to the tumor. This cuts off its blood supply and poisons it at the source. It’s not a cure, but it can shrink tumors and extend life by years.
Stage C (advanced): Cancer has spread to blood vessels or lymph nodes. Surgery and ablation won’t help. The main treatment is targeted drugs like sorafenib or lenvatinib. These block signals that help tumors grow. Immunotherapy combinations - like atezolizumab plus bevacizumab - are now first-line for many patients because they’ve shown better survival than older drugs. Median survival is 15-20 months, but some patients live much longer.
Stage D (end-stage): The liver is failing, and the cancer is widespread. At this point, treatment focuses on comfort. Liver transplant is the only potential cure, but only if the tumor is small enough and the patient is healthy enough to survive surgery. The Milan criteria - one tumor under 5 cm, or up to three tumors each under 3 cm - are still the standard for transplant eligibility.
The Real Barriers: Why People Miss Screenings
Guidelines are clear. But in practice, most people with cirrhosis never get screened. Why?- Doctors don’t trigger reminders. In 67% of clinics, there’s no electronic alert when a patient is diagnosed with cirrhosis. No reminder = no screening.
- Patient no-shows are high. Between 25% and 40% of people miss their ultrasound appointments. Some are scared. Others don’t understand why they need it if they feel fine.
- Access is unequal. Black patients are less than half as likely to get screened as white patients. Medicaid patients are screened at half the rate of those with private insurance.
- Cost and logistics. Ultrasound costs about $287 a year per patient. Add AFP testing, and it jumps to $412. For uninsured patients, that’s a lot. And not every clinic has a radiologist trained to read liver ultrasounds.
Successful programs fix these problems. One VA study used patient navigators - trained staff who call patients, schedule appointments, and explain why screening matters. No-show rates dropped from 32% to 14%. Another hospital added automated alerts to their electronic records. Time from cirrhosis diagnosis to first ultrasound dropped from 142 days to 67.
What’s Coming Next
The future of HCC screening is smarter, not just more frequent. New tools are on the horizon:- AI-assisted ultrasound: Tools like Medtronic’s LiverAssist (FDA-cleared in 2022) help technicians spot tiny tumors that humans might miss. They boost detection by 18-22%.
- Blood biomarkers: The GALAD score - which looks at gender, age, AFP, AFP-L3, and DCP - can detect early HCC with 85% accuracy. It’s not ready for prime time yet, but NIH-funded trials are testing it alongside imaging.
- Abbreviated MRI: A full liver MRI takes 30 minutes and costs $800+. New 5-7 minute protocols cut costs to $350-400. For high-risk patients, MRI may soon replace ultrasound.
- The aMAP score: A simple formula using age, gender, albumin, bilirubin, and platelets can predict risk with 81% accuracy. It’s being tested in Europe and Asia.
By 2027, experts predict that 30-40% of high-risk patients will get MRI instead of ultrasound. The AASLD is expected to update its guidelines in late 2024, and those updates will almost certainly push for risk-based screening.

What You Should Do Right Now
If you have cirrhosis:- Ask your doctor if you’re on a surveillance schedule. If not, ask why.
- Make sure your ultrasound is done every six months - no exceptions.
- Know your liver function score (Child-Pugh class). If you’re Class C, talk to your doctor about whether screening still makes sense.
- If you’re told you need a CT or MRI, don’t delay. Early detection saves lives.
- Bring someone with you to appointments. It’s hard to remember everything when you’re stressed.
If you’re a caregiver or family member: Help remind your loved one. Call to book the next scan. Drive them if they can’t. Write down questions before the visit. You’re not just helping - you’re extending their life.
Hepatocellular carcinoma doesn’t have to be a death sentence. But it won’t be caught unless someone is looking for it. The tools are here. The guidelines are clear. The only thing missing is action.
How often should someone with cirrhosis get screened for liver cancer?
Everyone with cirrhosis should get a liver ultrasound every six months. This is the standard recommendation from the American Association for the Study of Liver Diseases (AASLD) and the European Association for the Study of the Liver (EASL). Some newer guidelines suggest risk-based screening, where higher-risk patients may get MRI instead, but six-month ultrasound remains the baseline for most.
Is an AFP blood test enough to detect liver cancer?
No. AFP (alpha-fetoprotein) is not reliable on its own. It’s only elevated in about 60% of HCC cases, and it can rise for other reasons like hepatitis flare-ups or pregnancy. That’s why guidelines only recommend it as a supplement to ultrasound - not a replacement. An AFP level above 20 ng/mL should trigger further imaging, but a normal AFP doesn’t rule out cancer.
Can you survive hepatocellular carcinoma if it’s caught early?
Yes - and survival rates jump dramatically. When HCC is found at stage 0 or A (small, single tumors), treatments like radiofrequency ablation or surgery can cure the cancer in over 70% of cases. Five-year survival for early-stage HCC is 50-70%, compared to under 20% when caught late. That’s why surveillance is so critical.
Why don’t more people get screened for liver cancer?
There are many reasons. Many primary care doctors don’t have alerts in their electronic records to remind them to order screenings. Patients miss appointments due to fear, lack of transportation, or not understanding the risk. Insurance coverage varies, and some people can’t afford it. Racial and socioeconomic disparities are also significant - Black and Medicaid patients are screened at much lower rates than white and privately insured patients.
What’s the difference between ultrasound and MRI for HCC screening?
Ultrasound is the first-line tool - it’s cheaper, faster, and widely available. MRI is more sensitive and better at spotting small tumors and distinguishing between benign and cancerous nodules. But MRI costs more, takes longer, and isn’t always accessible. New abbreviated MRI protocols are changing that. For high-risk patients (like those with hepatitis B or advanced cirrhosis), MRI may soon replace ultrasound as the preferred screening tool.
Is liver transplant an option for hepatocellular carcinoma?
Yes - but only for a select group. The Milan criteria are used to determine eligibility: one tumor under 5 cm, or up to three tumors each under 3 cm, with no spread outside the liver. Transplant cures both the cancer and the cirrhosis. But waitlists are long, and patients must stay cancer-free while waiting. If the tumor grows beyond these limits, transplant is no longer an option.
What happens if I miss a screening appointment?
Missing one appointment doesn’t mean you’re doomed, but it increases your risk. HCC can grow quickly - sometimes doubling in size within six months. If you miss a scan, reschedule as soon as possible. Don’t wait until symptoms appear. Many people only get diagnosed after they feel pain or notice jaundice - and by then, treatment options are limited.
Next Steps if You’re at Risk
If you have cirrhosis from hepatitis B, hepatitis C, alcohol, or fatty liver disease:- Request a copy of your latest liver ultrasound report.
- Ask if your doctor uses a formal HCC surveillance protocol.
- Set a recurring calendar reminder for your next scan - six months from now.
- If you’re unsure about your risk level, ask for your Child-Pugh score and MELD score.
- Consider asking about the GALAD score or aMAP score if your clinic offers advanced testing.
Don’t wait for symptoms. By the time you feel sick, it’s often too late. Screening is the only thing standing between you and a late-stage diagnosis. It’s simple. It’s proven. And it’s your best shot at living longer.



Amy Ehinger
January 15, 2026 AT 20:16Just wanted to say I’m so glad this post exists. My mom has cirrhosis from years of heavy drinking, and she kept blowing off her ultrasounds because ‘she felt fine.’ We finally got her into a VA program with patient navigators, and they called her every week, drove her to appointments, even sent postcards. She had a 1.8 cm tumor caught last month - RFA worked like a charm. She’s back to gardening. I know it sounds cliché but screening really is the difference between ‘maybe next year’ and ‘I’m still here.’
Annie Choi
January 15, 2026 AT 22:58Guys listen up - this isn’t just medical advice it’s survival tech. Ultrasound every six months is non-negotiable. AFP is a noisy signal not a diagnostic tool. LI-RADS 5 = treat like your life depends on it because it does. MRI is the future for high risk. And if your doc doesn’t have an alert system? Fire them. Your liver doesn’t care about your doctor’s EHR limitations.
Arjun Seth
January 16, 2026 AT 12:42People are dying because they’re too lazy to get checked. I’ve seen this before. In my village in India, men with cirrhosis would drink until they collapsed - then blame the doctors. Screening? They say ‘God will decide.’ No. God gave us ultrasounds. Use them. Or stop pretending you care about your family. This isn’t complicated. Six months. One scan. No excuses.
Dan Mack
January 18, 2026 AT 04:55Let me guess - the pharmaceutical companies pushed this whole screening thing so they can sell you sorafenib at $12,000 a month. They don’t want you cured. They want you on lifelong chemo. And those ‘AI-assisted ultrasounds’? Probably just a data grab for Big Med. Why not just stop drinking and eat kale? That’s what they don’t want you to know.
Amy Vickberg
January 20, 2026 AT 01:00This is exactly the kind of clear, actionable info we need. I work in a community clinic and we’ve been struggling with no-show rates. I just shared this with our whole team. We’re implementing automated reminders next week. Also - if you’re reading this and you’ve missed a scan - it’s not too late. Just call. One call can change everything.
Jan Hess
January 21, 2026 AT 12:46My uncle got diagnosed with HCC last year after a routine scan. He’s 72. Had a transplant. Now he’s hiking again. People think liver cancer = death sentence. It’s not. It’s a race against time - and screening is your head start. Don’t wait for pain. Don’t wait for jaundice. Don’t wait for someone to die before you act. Do it now.
Gloria Montero Puertas
January 21, 2026 AT 21:03I’m sorry, but this entire post feels like a glossy brochure from a medical conglomerate. ‘Risk-based screening’? That’s just code for ‘we’re going to stop screening the poor.’ The AASLD guidelines are fine - but when Medicaid patients are screened at half the rate of privately insured? That’s not medical nuance. That’s systemic neglect. And you call this ‘actionable’? It’s a Band-Aid on a hemorrhage.
Tom Doan
January 22, 2026 AT 04:23Interesting. The data on AI-assisted ultrasound improving detection by 18-22% is compelling - but I’m curious: were the radiologists in those studies board-certified in hepatobiliary imaging? And was inter-observer variability accounted for? Also, the GALAD score’s validation cohort was predominantly Asian - how well does it generalize to African-American populations with high rates of NAFLD? This feels premature for widespread adoption.
Nishant Garg
January 23, 2026 AT 05:29In India, we have this saying: ‘The body doesn’t lie - but the doctor might.’ My father had cirrhosis. We couldn’t afford MRI. So we went to a government hospital where the ultrasound tech had been doing this for 30 years. He saw a nodule the machine missed. He said ‘This one’s bad.’ He was right. Tech helps. But human eyes? Still irreplaceable. Don’t forget that.
Nicholas Urmaza
January 24, 2026 AT 16:03If you have cirrhosis and you’re not getting screened every six months you’re playing Russian roulette with your liver. The stats don’t lie. Early detection = 70% five-year survival. Late detection = 15%. That’s not a gamble. That’s negligence. Stop making excuses. Book the scan. Bring your spouse. Write it in your planner. This isn’t optional. It’s mandatory for survival.
Sarah Mailloux
January 26, 2026 AT 05:07I’m a nurse in a rural clinic. We had one patient who missed three scans. We called her every time. She said ‘I’m fine.’ We sent a text: ‘We’re not asking you to believe in medicine. We’re asking you to believe in yourself.’ She showed up. Tumor found. Treated. Now she’s teaching other women in her church about screening. Small acts. Big ripples.
Nilesh Khedekar
January 28, 2026 AT 00:14Wow. This is the most honest, data-backed thing I’ve read in months. In India, we call cirrhosis ‘the silent thief’ - it steals your life slowly, quietly. No one talks about it. But here? People are screaming. And that’s good. Because silence kills. Screening isn’t just medicine - it’s rebellion against neglect. Thank you.
RUTH DE OLIVEIRA ALVES
January 29, 2026 AT 16:19It is imperative to underscore the significance of adherence to evidence-based surveillance protocols in patients diagnosed with cirrhosis. The absence of systematic implementation within primary care infrastructure represents a critical gap in preventive hepatology. Moreover, the persistent disparities in screening access among marginalized populations constitute a public health emergency requiring immediate policy intervention, equitable resource allocation, and culturally competent outreach strategies.