More than 1 in 10 people in the U.S. believe they’re allergic to a medication. But here’s the twist: most of them aren’t. A label like "penicillin allergy" often sticks for life-even when it’s wrong. And that mistake isn’t harmless. It leads to worse antibiotics, longer hospital stays, and thousands of extra dollars in medical bills every year. This isn’t just about a rash or a sneeze. It’s about how we misunderstand what a drug allergy really is-and which medications actually trigger real immune reactions.
Penicillin: The Most Misunderstood Drug Allergy
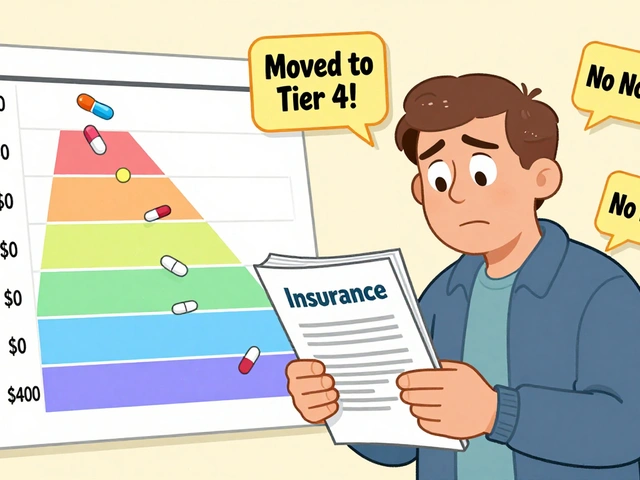
Penicillin is the big one. About 10% of Americans say they’re allergic to it. But studies show that over 95% of those people can take it safely after proper testing. Why? Because most reactions from decades ago were not true allergies. A skin rash after taking amoxicillin as a kid? That’s often just a viral rash. A stomach ache? That’s a side effect, not an allergy. True IgE-mediated penicillin allergy-a life-threatening reaction like anaphylaxis-is rare, affecting less than 1% of the population. Yet, people keep the label. And it costs the U.S. healthcare system over $1.2 billion annually because doctors avoid penicillin and reach for broader-spectrum antibiotics instead.
Here’s what actually happens in a real penicillin allergy: the immune system sees the drug as a threat. Within minutes, histamine floods the body. Swelling. Trouble breathing. Drop in blood pressure. That’s the danger. But here’s the good news: penicillin allergy testing is incredibly accurate. Skin testing combined with a small oral dose of amoxicillin predicts true allergy with 97-99% accuracy. If you were told you’re allergic as a child and never got tested, you might be able to take penicillin now. Many people outgrow it after 10 years without exposure.
Other Antibiotics That Trigger Reactions
Penicillin isn’t alone. Other beta-lactam antibiotics like cephalosporins and carbapenems can also cause allergic reactions-but cross-reactivity is much lower than people think. Older studies said 10% of penicillin-allergic people react to cephalosporins. Newer data shows it’s closer to 1-3%. That means if you’re allergic to penicillin, you’re probably fine with most cephalosporins. Still, doctors play it safe.
Sulfa drugs are another major player. Trimethoprim-sulfamethoxazole (Bactrim) is commonly prescribed for urinary tract infections and pneumonia. About 3% of the general population has a reaction to sulfa drugs. But for people with HIV, that number jumps to 60%. The reaction isn’t always immediate. It can show up as a rash, fever, or even organ inflammation days or weeks later. This is why doctors are extra cautious with sulfa drugs in immunocompromised patients.
NSAIDs: More Than Just a Headache
Nonsteroidal anti-inflammatory drugs like ibuprofen, naproxen, and aspirin are among the most common triggers of drug hypersensitivity. But these reactions are different. They don’t involve IgE antibodies. Instead, they mess with the body’s inflammatory pathways. This is why you might hear about aspirin-exacerbated respiratory disease (AERD). It’s not a typical allergy. It’s a condition where people with asthma or nasal polyps get severe breathing problems after taking aspirin or other NSAIDs. About 7% of adults with asthma and 14% with nasal polyps have this.
For most people, an NSAID reaction looks like hives, swelling, or wheezing within an hour. It’s not rare. One study found that for every 100 people who take NSAIDs, one will have a true hypersensitivity reaction. That’s why some people avoid all NSAIDs after one bad experience. But here’s the thing: if you reacted to ibuprofen, you might still be able to take naproxen-or even aspirin. The reactions aren’t always cross-reactive. Testing isn’t routine, but if you’ve had a serious reaction, seeing an allergist could open up pain relief options you didn’t know you had.
Anticonvulsants and the Genetic Risk
Some drug allergies aren’t random. They’re written in your DNA. Carbamazepine (Tegretol), used for epilepsy and nerve pain, can trigger Stevens-Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN)-life-threatening skin reactions. In Southeast Asian populations, a gene called HLA-B*1502 makes this risk 100 times higher. The FDA recommends testing for this gene before prescribing carbamazepine to people with ancestry from Thailand, Malaysia, or the Philippines. In Taiwan, where testing became routine, SJS/TEN cases dropped by 90%.
Lamotrigine (Lamictal) is another anticonvulsant that causes rash in 5-10% of users. Most are mild. But in 1 out of every 1,000 patient-years, it can lead to SJS. That’s why doctors start with low doses and increase slowly. If you get a rash while on lamotrigine, don’t ignore it. Call your doctor immediately. A delayed rash-appearing 10 to 14 days after starting the drug-is a red flag.
Chemotherapy and Biologics: The New Frontiers
Cancer drugs are notorious for causing hypersensitivity. Taxanes like paclitaxel (Taxol) trigger reactions in up to 41% of patients. Symptoms? Flushing, low blood pressure, chest tightness-often during the infusion. Monoclonal antibodies like cetuximab (Erbitux) are even trickier. They can cause anaphylaxis in 2% of patients. The good news? Hospitals have protocols. Premedication with steroids and antihistamines cuts severe reactions by over 90%. Desensitization-giving the drug in tiny, slowly increasing doses-is now standard for patients who need these drugs but have had reactions before.
And it’s getting worse. Biologics-drugs made from living cells-are growing fast. They’re powerful, but they’re also more likely to trigger immune reactions. Experts predict we’ll need 20% more allergists by 2030 just to handle the influx.
Radiation Dyes and the Silent Risk
When you get an MRI or CT scan with contrast dye, you’re not just getting a picture-you’re getting a potential reaction. About 1-3% of patients have some kind of reaction: nausea, itching, hives. Severe reactions are rare-only 0.01% to 0.04%-but they happen. The good news? If you’ve had a reaction before, premedication with steroids and antihistamines drops your risk of another moderate or severe reaction from 12.7% down to just 1%. Many hospitals now screen for prior reactions and pre-treat accordingly.

How to Know If It’s Real
Not every bad reaction is an allergy. Here’s how to tell:
- True allergy: Happens within minutes to hours. Involves immune system. Symptoms: hives, swelling, trouble breathing, anaphylaxis.
- Side effect: Nausea, dizziness, headache. Common. Predictable. Not immune-related.
- Delayed reaction: Rash, fever, joint pain appearing days later. Could be allergic or just a drug response. Needs evaluation.
- Drug interaction: Reaction caused by mixing two medications. Not an allergy.
If you’ve had a serious reaction, don’t assume it’s permanent. Many people are mislabeled. A proper allergy evaluation includes:
- A detailed history of your reaction
- Skin testing (for penicillin and some other drugs)
- A supervised oral challenge (taking the drug again under medical supervision)
Penicillin testing takes 2-4 hours. It’s safe. And it’s accurate. If you’re told you’re allergic but never got tested, you might be one of the 80% who can safely take penicillin now.
What You Can Do
Stop assuming your allergy label is set in stone. If you were told you’re allergic to a drug as a child, ask: Did I ever get tested? Did I have a true anaphylactic reaction? Was it documented? If not, talk to your doctor about a referral to an allergist. Many insurance plans cover testing, especially if you’re on multiple medications or need antibiotics often.
Also, update your medical records. If you’ve been told you’re allergic to penicillin but later found out it was wrong, make sure your primary care doctor and pharmacist know. Electronic health records still carry old labels-even when they’re inaccurate. That’s how people end up with unnecessary antibiotics.
And if you’re taking carbamazepine, lamotrigine, or any chemotherapy drug and develop a rash-no matter how mild-call your doctor. Don’t wait. Delayed reactions can turn deadly.
Why This Matters
Drug allergies aren’t just about discomfort. They shape how we treat infections, manage pain, fight cancer, and control seizures. Mislabeling leads to antibiotic resistance, longer hospital stays, and higher costs. It also means people miss out on the best, safest, and cheapest treatments. A penicillin allergy label might seem harmless. But it’s one of the most common-and dangerous-medical misdiagnoses out there.
Knowledge is power. And testing? It’s the key to unlocking better care.
Can you outgrow a drug allergy?
Yes, especially with penicillin. Studies show that 80% of people who had a penicillin allergy label as children lose their sensitivity after 10 years without exposure. The immune system can forget the false alarm. That’s why retesting is so important-especially if you need antibiotics for an infection.
Is a rash always a sign of drug allergy?
No. Many rashes from medications are not allergic. Viral infections, especially in kids, can cause rashes right after taking antibiotics. This is often mistaken for an allergy. True allergic rashes usually appear within hours, are itchy, and may be accompanied by swelling or breathing issues. Delayed rashes (after 7+ days) can still be serious but need careful evaluation to rule out other causes.
Can you have a reaction to a drug you’ve taken before without problems?
Yes. The immune system can suddenly start reacting after multiple exposures. This is common with drugs like vancomycin, chemotherapy agents, and biologics. The first few times, you might feel fine. Then, out of nowhere, you get hives or low blood pressure. That’s why medical teams monitor infusions closely-even for drugs you’ve taken before.
Are there tests for all drug allergies?
No. Reliable tests exist only for a few drugs: penicillin, some cephalosporins, insulin, and certain chemotherapy agents. For most others-like sulfa drugs, NSAIDs, or anticonvulsants-there’s no blood or skin test. Diagnosis relies on your history, timing of the reaction, and sometimes a supervised challenge. That’s why detailed records of your reaction are so important.
What should I do if I think I’m allergic to a medication?
Don’t just stop taking it and assume the label is correct. Write down exactly what happened: when, what symptoms, how long they lasted, and if you’ve taken it again since. Then ask your doctor for a referral to an allergist. Many hospitals now offer penicillin allergy clinics. Testing is quick, safe, and can change your treatment options for life.






Alex Ogle
February 7, 2026 AT 15:49So I’ve been thinking about this for a while. My mom was told she was allergic to penicillin when she was six-rash after amoxicillin, no anaphylaxis, no doctor follow-up. Decades later, she needed antibiotics for a UTI, and her doctor insisted on something way more expensive and broader-spectrum. She ended up with a yeast infection, a week of nausea, and a $900 bill. Then, out of nowhere, she found a clinic that does penicillin testing. Two hours later? She could take it. No reaction. No drama. Just… relief. I didn’t even know this was a thing. Why isn’t this standard? Why do we still treat allergy labels like sacred texts? It’s wild that we’re spending billions on unnecessary antibiotics because we’re too lazy to test.
Chima Ifeanyi
February 7, 2026 AT 22:00The data here is statistically significant but methodologically flawed. You’re conflating IgE-mediated hypersensitivity with non-IgE-mediated immune dysregulation, which fundamentally undermines the clinical utility of your assertions. Moreover, the 95% ‘outgrowing’ statistic is drawn from retrospective cohort studies with selection bias-patients who sought retesting were already predisposed to believe they were misdiagnosed. The real issue is not mislabeling, but the absence of standardized, population-wide immunophenotyping protocols. Until we implement HLA typing and basophil activation testing at scale, we’re just rearranging deck chairs on the Titanic.
Ashlyn Ellison
February 8, 2026 AT 10:03My kid got a rash on amoxicillin at age 3. We thought it was an allergy. Turned out it was roseola. Never got tested. Now I’m 32, got a sinus infection, and my doctor gave me azithromycin because ‘penicillin allergy.’ I asked if I could get tested. He said, ‘Eh, probably not worth it.’ So I went to an urgent care. Paid $120. Got cleared in 90 minutes. Now I’m on penicillin. Saved $600 on antibiotics alone. Why is this so hard?
Frank Baumann
February 10, 2026 AT 06:20Let me tell you about my cousin. She had a reaction to sulfa drugs after a UTI. Didn’t know it was delayed. Thought it was ‘just a rash.’ Three weeks later, she ended up in the ICU with Stevens-Johnson. Burned 40% of her skin. Lost her nails. Couldn’t eat for months. They had to do skin grafts. She’s fine now. But she’ll never take sulfa again. And you know what? She shouldn’t. Not because of some vague ‘maybe’-because she lived it. You can’t just say ‘test it’ like it’s a software bug. Some people don’t get a second chance. This isn’t a spreadsheet. It’s a human body.
Random Guy
February 11, 2026 AT 19:23penicillin allergy? more like penicillin drama. everyone and their dog thinks they're allergic. i had a rash once. now i'm 'allergic' to 7 drugs. my pharmacist has a shrine to me. i'm basically a walking medical myth. next thing you know, i'll be allergic to oxygen.
Brett Pouser
February 13, 2026 AT 12:44As a Nigerian-American, I’ve seen both sides. In Nigeria, we rarely test for drug allergies-cost, access, infrastructure. But here? We over-test, over-label, over-fear. My uncle in Lagos got penicillin for pneumonia. No issues. My cousin here got flagged for ‘allergy’ after a rash, then got put on vancomycin for a UTI. Cost? $4,000. Side effects? Diarrhea for two weeks. The system is broken. We need to stop treating every rash like a death sentence. And we need to stop pretending culture doesn’t matter in medicine.
Karianne Jackson
February 14, 2026 AT 10:51I got a rash on amoxicillin. I cried. I thought I was gonna die. Now I know it was just a virus. But I still don’t take it. I’m scared. It’s not about logic. It’s about fear. And that’s real.
Chelsea Cook
February 16, 2026 AT 04:01So let me get this straight-you’re telling me I could’ve been taking the best antibiotic for my infections for the last 15 years… but I didn’t because someone scribbled ‘allergy’ on a chart in 1998? And now we’re paying billions because we’re too scared to ask a simple question? I’m not mad. I’m just… disappointed. This isn’t science. It’s folklore with a price tag.
Andy Cortez
February 16, 2026 AT 05:59you people are so gullible. 'penicillin allergy'? more like 'penicillin fear'. they're just scared of the word 'allergy' like it's a curse. i've taken penicillin 5 times. no problem. you think your body's a magic box? no. it's biology. stop being dramatic. also, why is everyone so obsessed with penicillin? what about the 100 other drugs no one talks about? you're all just chasing headlines.
Andrew Jackson
February 16, 2026 AT 18:33It is a moral failure of Western medicine that we allow anecdotal, non-validated, pediatric-era labels to dictate therapeutic decisions for adults. This is not medical practice-it is superstition codified in electronic health records. The erosion of clinical judgment in favor of algorithmic risk aversion has led to a cascade of iatrogenic harm. Furthermore, the financial incentives for prescribing broad-spectrum antibiotics-driven by pharmaceutical marketing and hospital formularies-exacerbate this crisis. We must return to evidence-based, patient-centered care, not the bureaucratic cowardice masquerading as safety.
Joseph Charles Colin
February 18, 2026 AT 18:25Important clarification: The 97-99% accuracy of penicillin skin testing applies only to immediate-type (IgE-mediated) reactions. Delayed rashes, drug-induced lupus, or serum sickness are not detectable via skin tests. Additionally, cross-reactivity between penicillins and cephalosporins is not binary-it’s a spectrum based on R-group side chains. Cefazolin has higher cross-reactivity than ceftriaxone. The literature is nuanced, but most guidelines oversimplify. Also, for carbamazepine, HLA-B*1502 screening is mandatory in Southeast Asia, but not in the U.S. unless the patient has ancestry from those regions. That’s a gap in care.
John Sonnenberg
February 20, 2026 AT 01:34Let me just say this: I had a reaction to ibuprofen. Swelling. Hives. Felt like I was dying. I went to the ER. They said, ‘It’s probably not an allergy.’ I said, ‘I don’t care. I’m never taking it again.’ Now I take naproxen. No problem. But I still won’t touch ibuprofen. Not because of science. Because I remember the fear. And if you’ve ever felt your throat close up-you get it. You don’t need a test. You need to live it.
Joshua Smith
February 22, 2026 AT 00:19I’m a nurse. I’ve seen this over and over. A patient comes in with a penicillin allergy label. We check their chart. No documentation of a real reaction. No anaphylaxis. Just ‘rash as a kid.’ We offer testing. 80% say no. Why? ‘I don’t want to risk it.’ I get it. But then they get a different antibiotic, get sicker, stay longer, spend more. It’s heartbreaking. We need to make testing easier. Maybe even automatic-like flu shots. If you’ve got a label older than 10 years, you get a referral. No questions. Just care.
Jessica Klaar
February 23, 2026 AT 01:30I’m a single mom. My daughter had a rash on amoxicillin. We didn’t think much of it. Years later, she needed antibiotics for pneumonia. I refused to let her take penicillin. We ended up in the hospital for three days because the ‘safe’ antibiotics didn’t work. I cried in the parking lot. I felt like a bad mom. I wish someone had told me-back then-that it might not have been an allergy. That testing exists. That it’s safe. That it’s covered by insurance. I’m not angry. I’m just… so tired. And I wish someone had held my hand and said, ‘It’s okay to ask.’