Medication Communication: How to Talk to Your Doctor About Drugs Safely
When you take a medication, medication communication, the clear, two-way exchange between patients and providers about drug use, risks, and side effects. Also known as drug dialogue, it’s not just about following instructions—it’s about understanding why you’re taking something, what could go wrong, and how to act if it does. Too many people stay silent when they’re confused, scared, or embarrassed. That silence is what turns a simple mix-up into a hospital visit. A 2023 study in the Journal of Patient Safety found that over 40% of medication errors could have been prevented if patients had asked one clear question before leaving the clinic.
medication errors, mistakes in prescribing, dispensing, or taking drugs that cause harm happen because of gaps in this conversation. Maybe your doctor didn’t explain the black box warning on your blood thinner. Maybe the pharmacist didn’t catch that your fish oil and aspirin could add up. Maybe you didn’t say you’ve been skipping doses because depression made you feel hopeless. These aren’t just mistakes—they’re failures of communication. And they’re fixable.
Good patient-provider communication, the structured, honest exchange that ensures treatment matches real-life needs means asking: "What happens if I miss a dose?" "Is this the only option?" "What signs mean I need to call right away?" It means bringing your pill bottles to every appointment. It means saying, "I didn’t take this because it made me dizzy," instead of pretending everything’s fine. The tools exist—barcode scanning in pharmacies cuts errors by 93%, but only if the patient tells the pharmacist about the new supplement they started. INR monitoring works only if you report your diet changes. Peak flow tracking helps only if you tell your doctor when your numbers drop.
And it’s not just about the pills. It’s about the stories behind them. Someone skipping their diabetes meds because they can’t afford them. Someone afraid to mention their depression because they think it’s "not medical." Someone confused why their generic drug looks different this month. These aren’t edge cases—they’re everyday realities. The posts below cover how to spot when communication breaks down, how to report a mistake without fear, how to understand warnings on your bottle, and how to handle interactions between common drugs like blood thinners and supplements. You’ll find real stories, step-by-step guides, and the exact phrases to use with your provider. No jargon. No fluff. Just what you need to stay safe.
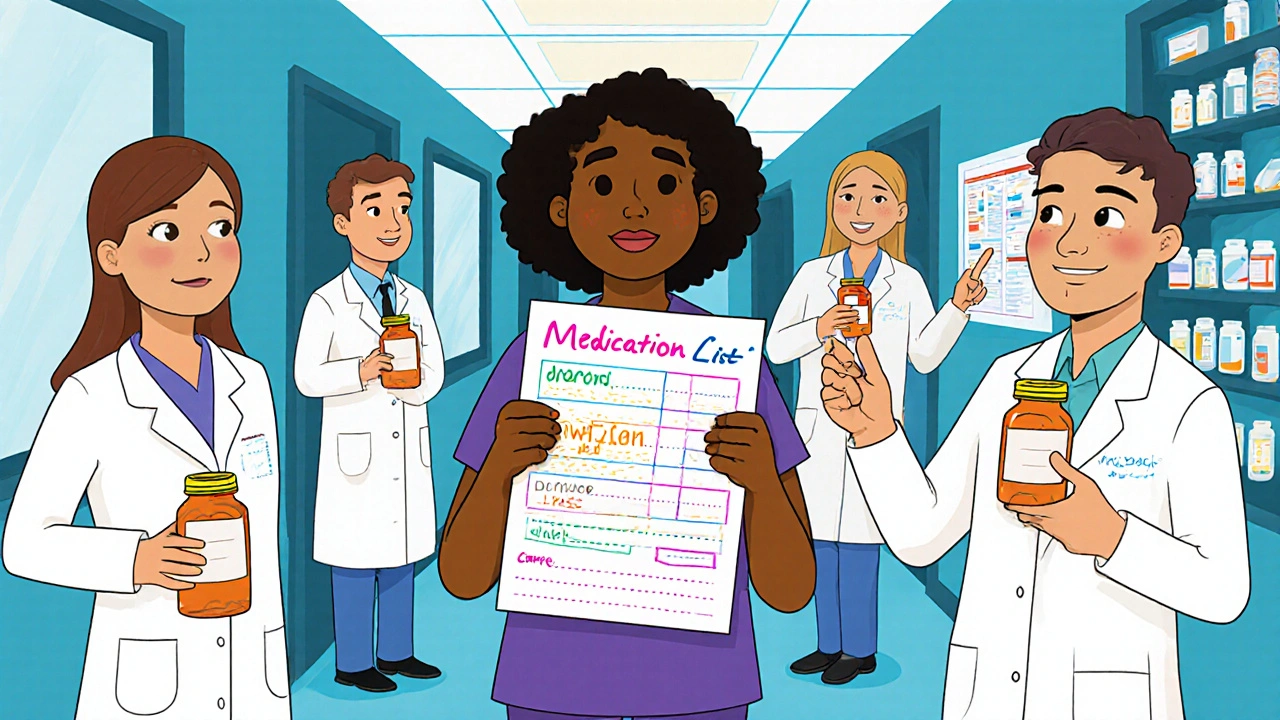
How to Communicate with Multiple Healthcare Providers About Your Medications
Learn how to prevent dangerous medication errors by communicating clearly with multiple healthcare providers. Get practical steps to track your meds, work with your pharmacist, and ensure all your doctors are on the same page.