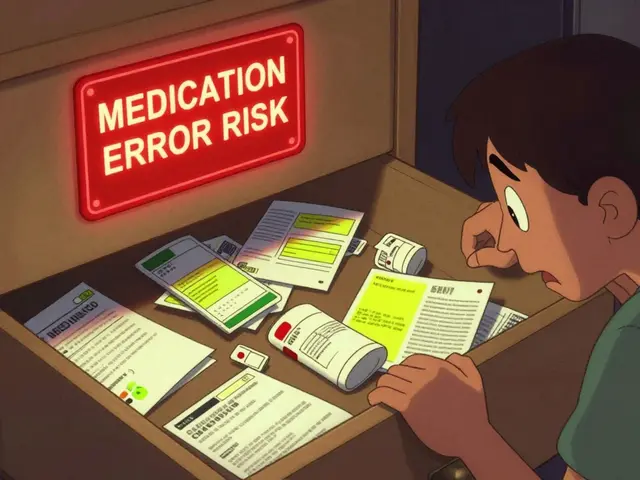
Imagine this: you’re seeing three different doctors for separate conditions. One prescribes a new painkiller. Another adds a blood pressure pill. A third gives you an antidepressant. None of them know what the others prescribed. A month later, you end up in the ER because the mix of drugs caused dangerous side effects. This isn’t a rare story. It happens more often than you think.
Why Medication Communication Between Providers Matters
Every year in the U.S., over 1.5 million people are harmed by medication errors. About 7,000 of those cases result in death. A lot of those errors aren’t because doctors made a mistake-they’re because no one told the right person what was being prescribed. When you have multiple providers, each one focuses on their own piece of your health. A cardiologist looks at your heart. A rheumatologist looks at your joints. A psychiatrist looks at your mood. But only you carry the full picture. If those providers don’t talk to each other, your medications can clash, overlap, or cancel each other out. Research from the University of Ottawa shows that medication communication isn’t just part of care-it’s a separate, critical activity. It’s not enough to just write a prescription. Someone has to make sure everyone involved knows what’s been written, why, and how it fits with everything else.The Four Essentials of a Complete Medication List
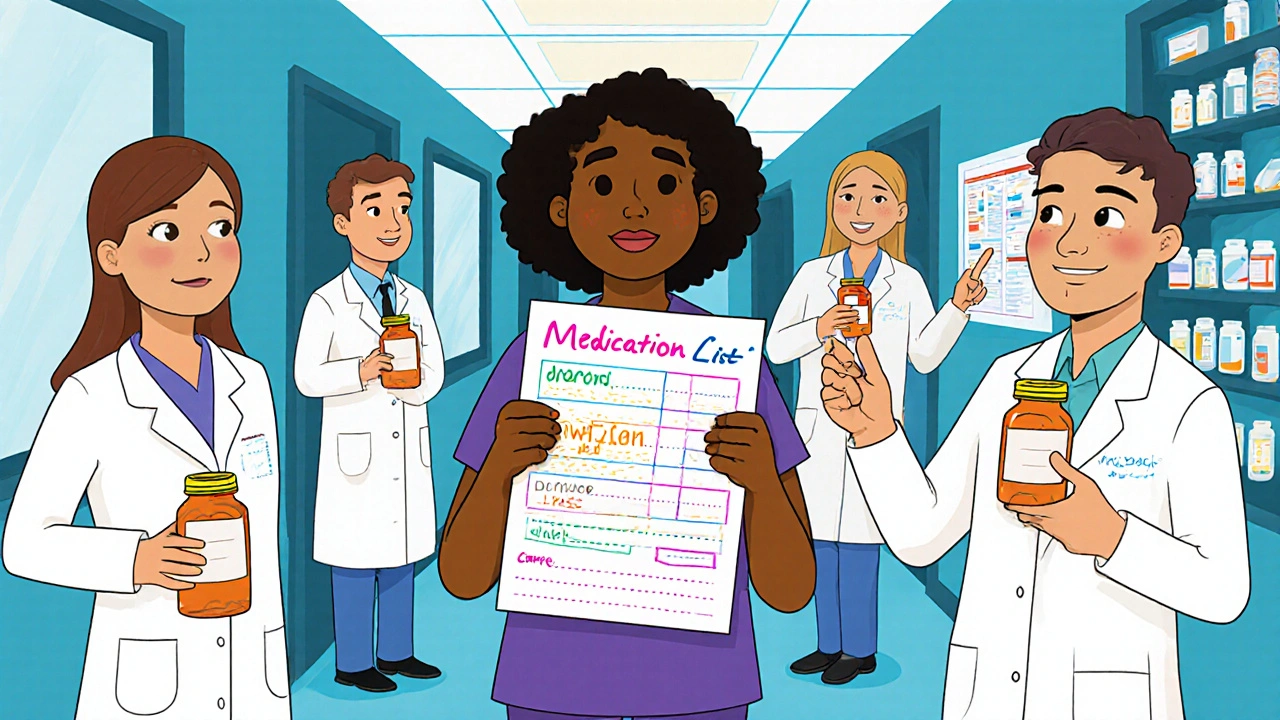
The simplest, most powerful tool you can use is a current, accurate list of every medication you take. Not just the name. Not just the dose. You need all four key pieces:- Name of the medication (including brand and generic if applicable)
- Dosage (e.g., 10 mg, 500 mg)
- Frequency (e.g., once daily, twice a week, as needed)
- Purpose (e.g., “for high blood pressure,” “for anxiety,” “for pain”)
Who Should Be Talking to Whom?
You’re not just a patient-you’re the hub of your own care team. The people who need to communicate include:- Your primary care provider (PCP)
- Specialists (cardiologist, endocrinologist, neurologist, etc.)
- Your pharmacist
- Nurses and care coordinators
- Family members or caregivers who help you manage meds
How to Make Sure Providers Actually Talk
You can’t force doctors to talk to each other. But you can make it easier for them. Ask for a care summary after every specialist visit. Most clinics can generate a summary report. Request it in writing or ask for an electronic copy to be sent to your PCP. Use a shared electronic health record (EHR) if possible. If your PCP and specialists are part of the same health system, chances are they can see each other’s notes. But if you’re seeing providers across different hospitals or clinics, that’s not guaranteed. A 2023 report found only 38% of providers can access full medication histories across systems. Bring your list to every appointment-even if you think they already have it. Providers are busy. Systems glitch. Paperwork gets lost. Your list is your backup. Use the Teach-Back Method. After a provider explains a new medication, say: “Just to make sure I got it right, can you help me explain how to take this?” If you can repeat the instructions back clearly, you’re far less likely to make a mistake. Studies show this reduces misunderstandings by 45%.
Track What’s Working (and What’s Not)
Medications don’t just work or not work-they cause side effects. Some are obvious. Others are subtle: fatigue, brain fog, dizziness, changes in sleep or appetite. Start a simple health journal. For each medication, write down:- When you started it
- Any side effects you notice
- How you’re feeling overall
- Whether you’ve missed any doses
What to Do When Things Go Wrong
If you’ve had a bad reaction, missed a dose, or think your meds are conflicting, don’t wait. Act. Call your pharmacist first. They can quickly check for interactions and tell you if it’s an emergency. Many have 24/7 hotlines. Don’t stop a medication on your own. Even if you think it’s causing a problem, stopping suddenly can be dangerous. Talk to your provider first. Request a medication reconciliation. This is a formal review of all your meds, usually done during hospital discharge or after a major change. Ask your PCP to schedule one if you’ve seen multiple providers recently.Why Integrated Care Works Better
Patients in Accountable Care Organizations (ACOs) or integrated health systems have better outcomes. Why? Because communication is built into the system. CMS data shows ACO patients have 27% fewer medication-related hospital readmissions. Why? Because primary care doctors and specialists are on the same team. They share records. They hold regular care coordination meetings. They’re incentivized to keep you out of the hospital. If you’re on Medicare, ask if your plan is part of a Shared Savings Program. You’re more likely to get coordinated care. Even if you’re not in an ACO, you can still push for it. Say to your PCP: “I see three specialists. Can we set up a care coordination plan?” Many practices now have care coordinators whose job is exactly that.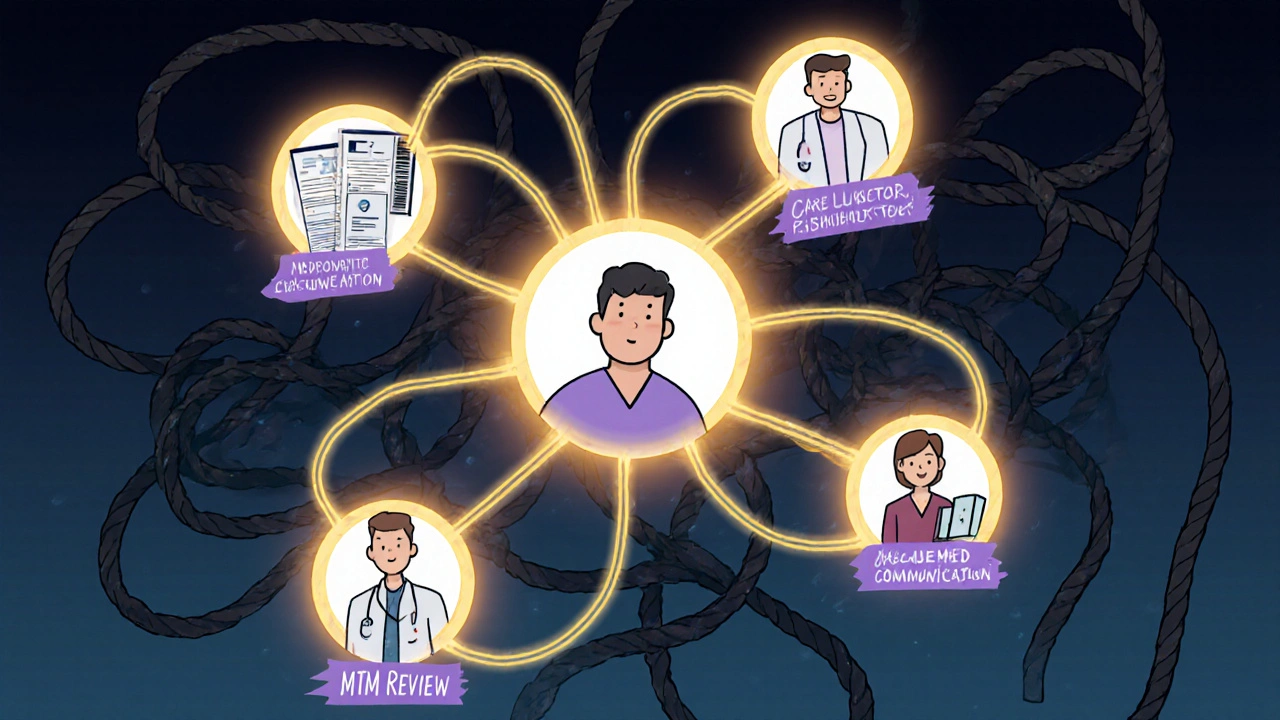
The Future Is Here-And It’s Pharmacists
The biggest shift in medication communication isn’t coming in five years. It’s happening now. More than 78% of independent pharmacies will offer formal Medication Therapy Management services by 2025. That means your pharmacist can:- Review all your meds in one place
- Call your doctors to clarify prescriptions
- Send you alerts about interactions
- Work with your care team as a full member
Start Today: Your Action Plan
You don’t need to fix everything at once. Start here:- Make or update your four-element medication list right now. Include every pill, patch, injection, and supplement.
- Print two copies. Keep one at home. Bring one to your next appointment.
- Call your pharmacy and ask if they offer Medication Therapy Management (MTM). If yes, schedule a free review.
- Next time you see a specialist, say: “Can you please send a summary of my new prescriptions to my primary care doctor?”
- Start a simple journal. Note any new side effects or changes in how you feel.
Don’t Assume They’re Talking
The biggest myth in healthcare is that your doctors talk to each other. They don’t. Not unless you make sure they do. You’re the only person who sees the full picture. You’re the only one who knows how you feel after taking all those pills. Don’t wait for someone else to fix the gaps. Be the bridge. Your health isn’t a puzzle with pieces scattered across different tables. It’s one picture-and you’re the only one holding all the pieces.What should I do if my doctors prescribe conflicting medications?
Don’t stop any medication on your own. First, call your pharmacist-they can check for dangerous interactions immediately. Then, schedule a medication review with your primary care provider. Bring your updated medication list and ask them to coordinate with your specialists. If needed, request a formal medication reconciliation, especially after hospital visits or major changes in care.
Do all my doctors have access to each other’s records?
Not necessarily. If all your providers are in the same health system, they likely can. But if you see doctors at different hospitals or clinics, their electronic records may not connect. Only 38% of providers can access full medication histories across different systems. Always bring your own updated medication list to every appointment.
How can a pharmacist help me manage multiple medications?
Pharmacists are medication experts trained to spot interactions, duplications, and dosing errors. Many offer free Medication Therapy Management (MTM) services, where they review all your meds, call your doctors to clarify prescriptions, and help you understand what each one does. Patients who use these services have 32% higher adherence and 63% higher confidence in their treatment plans.
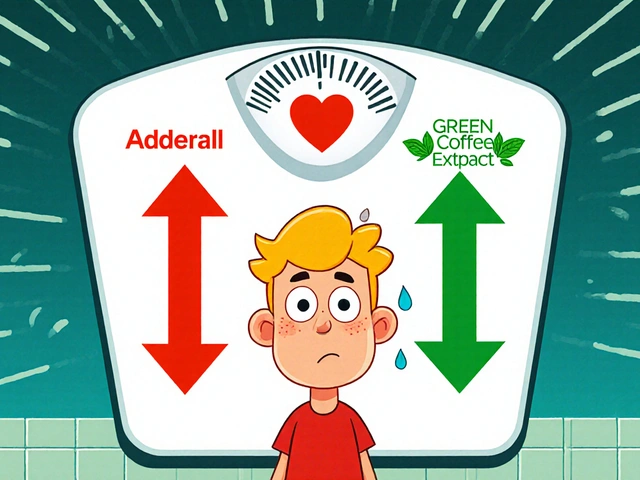
Is it safe to take supplements with my prescription meds?
Not always. Many supplements interact with prescription drugs. For example, St. John’s Wort can reduce the effectiveness of blood thinners and antidepressants. Always tell your pharmacist and doctor about every supplement you take-even if you think it’s “natural” or “harmless.” Include them on your medication list.
How often should I update my medication list?
Update it every time you start, stop, or change the dose of any medication-even if it’s temporary. Also update it after every specialist visit, hospital discharge, or pharmacy refill. Keep a printed copy in your wallet and a digital copy on your phone. Use it at every appointment.
What if I feel overwhelmed managing so many medications?
You’re not alone. Over half of elderly patients say they feel overwhelmed. Start by simplifying: ask your pharmacist if any meds can be combined or taken less often. Use a pill organizer. Set phone reminders. Ask your primary care provider for a care coordination plan. You don’t have to manage this alone-there are systems and people ready to help.




Rachel Wusowicz
November 15, 2025 AT 16:08So... let me get this right: you're telling me that the entire U.S. healthcare system is just a glorified game of telephone-where the last person to hear the message is the one who gets the overdose?? And we're supposed to trust these people with our lives?? I mean, I've seen the documentaries... the corporate hospitals are literally designed to keep you sick so they keep billing... and now you want me to believe that if I just print out my meds list, everything will be fixed??
Where's the whistleblower testimony?? Where's the leaked memo from Big Pharma about keeping patients confused?? I've got 17 pills a day, and I swear three of them are just placebos with a $400 price tag... and no one's asking why the pharmacist won't look me in the eye anymore... I'm not paranoid-I'm just observant.
They don't want you to know that your EHR is just a marketing tool... the real data is stored in off-shore servers... and your doctor doesn't even see your full record unless you pay for the "premium access" upgrade... I found a PDF buried in my portal that said "Data Silos: Strategic Advantage"... I think I'm being gaslit by algorithms...
And don't get me started on the pharmacists... they're just corporate agents in white coats... I asked mine about St. John's Wort and she looked at me like I'd just confessed to a crime... then she handed me a coupon for a new antidepressant... I'm not crazy-I'm just the only one paying attention.
Someone needs to sue the AMA... and maybe start a podcast... I've got 12 hours of audio recordings of my doctors mumbling about "protocols" while I hold up my list... they're terrified of transparency... I'm just the inconvenient truth with a printer.
Bring your list? Please. My list is 17 pages long and includes the brand names, generic names, batch numbers, expiration dates, and the emotional toll of each pill... and no one in the system can even open a PDF without crashing their system... I've been told to "just use the app"... but the app requires a password, a fingerprint, a retinal scan, and a notarized affidavit... I'm not a patient-I'm a data point with anxiety.
And the "care coordinator"? That's just a title for the intern who's supposed to call everyone but never does... I've emailed them 19 times... they auto-replied with a link to a 47-page PDF titled "How to Ask Better Questions"... I think I'm being punished for being too competent.
So yes-I bring my list. I print it in triplicate. I laminated it. I keep one in my bra, one in my shoe, and one in a sealed envelope under my mattress... because if I die, I want someone to know who really killed me.
Dan Angles
November 17, 2025 AT 09:37Thank you for this meticulously researched and clinically grounded exposition. The statistical references to the 1.5 million annual medication error incidents in the U.S., as corroborated by the Institute of Medicine and the Agency for Healthcare Research and Quality, underscore an urgent systemic imperative that extends beyond individual patient responsibility.
It is imperative to recognize that while patient engagement is a necessary component of medication safety, it is not sufficient. The structural fragmentation of care delivery, the absence of interoperable electronic health records across vendor platforms, and the disincentivization of inter-provider communication within fee-for-service reimbursement models are the true root causes.
The proposed action plan-while practical and commendable-is a band-aid on a hemorrhage. The only sustainable solution lies in federal legislation mandating interoperability standards, funding for health information exchanges, and the integration of clinical pharmacists as licensed members of the care team under Medicare and Medicaid.
Furthermore, the Teach-Back Method, though empirically validated, should not be the burden of the patient to initiate. It must be codified as a standard of care, with documentation requirements and quality metrics tied to provider reimbursement.
Patients should not be expected to serve as de facto care coordinators. This is a failure of professional accountability, not patient negligence. The onus must shift from the individual to the institution.
I urge all clinicians, administrators, and policymakers to treat this not as a behavioral issue, but as a systemic one requiring structural reform. The data is clear. The solutions are known. What is lacking is the political will.
David Rooksby
November 18, 2025 AT 10:43Oh wow, so we're just supposed to carry around a little paper list like we're in 1998 and doctors still use fax machines? LOL. Newsflash: my GP's computer system crashed last week and they lost my entire med history for three days-three days!-and my blood pressure spiked because they couldn't remember if I was on lisinopril or ramipril. I had to call my pharmacist and read it out loud to them while they typed it into their ancient system.
And don't even get me started on the "pharmacist" thing. My local chemist is a guy who graduated in 2005 and still thinks "as needed" means "whenever I feel like it." He once told me to take my antidepressant with a beer "to make it work better." I swear to god, I almost called the police.
And the EHRs? Ha! My cardiologist is in one system, my neurologist in another, my psychiatrist in a third, and my GP uses a program that looks like it was coded in Notepad by a 14-year-old. I asked if they could "sync" and they laughed. Said "we're not Google."
Meanwhile, my meds cost more than my rent. I take 11 pills a day. One of them is for a condition I don't even have anymore. I asked to stop it. They said "we'll review it next quarter." Next quarter is in 2027. I'm 38. I don't have that long.
And yeah, I keep a list. I have a spreadsheet. I have a Google Doc. I have it on my phone, my tablet, my smartwatch, and I've emailed it to my dog's collar. I'm the only one who cares. Everyone else is too busy being paid by the pill.
Also, I think the government is using my meds to track my emotions. I swear my antidepressant makes my phone autocorrect "hello" to "they're watching."
Melanie Taylor
November 19, 2025 AT 06:27OMG YES THIS!!! 🙌 I've been doing the list thing for years and it's literally saved my life! 💖 I even color-coded my meds by purpose-blue for heart, green for brain, pink for pain, and yellow for "don't touch unless you want to cry" 😅
My pharmacist is my angel. She called my doctor last month because my blood thinner was conflicting with my new turmeric supplement (who knew??) and now she sends me little texts like "Hey, your pill schedule changes tomorrow! Don't forget!" 💌
And I started my journal! I write down every weird feeling-like when I felt like my tongue was made of cotton after the new anxiety med. My doctor was SO impressed. She said, "You're the only patient who actually tells me what's happening." 🥹
Bring your list. Use the app. Ask the pharmacist. Say "teach back" like a boss. You're not being annoying-you're being a superhero. 💪❤️
Teresa Smith
November 21, 2025 AT 05:26This is not merely a logistical issue-it is an ethical imperative. The fragmentation of care is a moral failure of the medical-industrial complex. Patients are being asked to perform labor that should be performed by trained professionals, and this is not empowerment-it is exploitation.
That said, the action plan outlined here is a necessary and courageous act of resistance. The medication list is not a tool-it is a weapon against neglect. The journal is not a diary-it is a forensic record. The pharmacist consultation is not a service-it is a right.
Every time a patient brings their list, they are asserting their personhood in a system that reduces them to a code. Every time they ask for a care summary, they are demanding dignity. Every time they say, "I need a reconciliation," they are refusing to be disposable.
And yet, the burden remains disproportionate. Those with time, literacy, access, and social capital can navigate this. Those without? They die quietly in emergency rooms, their names never recorded, their medications never reconciled.
This is not about individual responsibility. It is about collective accountability. We must demand that systems be designed for the patient-not the profit margin. And until then, we must be the bridge. Because no one else will.
ZAK SCHADER
November 21, 2025 AT 21:09lol why are we even talking about this? doctors dont care. they just wanna get paid. i got 12 pills a day and half of em are for side effects from the other half. i asked my doc why and he said "that's just how it is."
and the "pharmacist"? they dont even know my name. i've been going there for 5 years and they still call me "sir" even though i'm a woman.
and dont get me started on the "ehealth" thing. my records are all over the place. i had to pay $45 to get my own lab results from my own hospital. thats not healthcare. thats extortion.
so yeah. bring your list. but dont expect anyone to care. they're all just here for the paycheck.
Danish dan iwan Adventure
November 22, 2025 AT 08:37Medication reconciliation is a foundational pillar of pharmacovigilance. Inadequate polypharmacy oversight leads to iatrogenic cascades. The 37% reduction in adverse events correlates directly with structured medication documentation, per Tulane’s 2021 cohort analysis. Pharmacist-led MTM interventions demonstrate statistically significant improvements in adherence (p<0.01) and therapeutic alignment. The absence of EHR interoperability remains a critical systemic vulnerability. Patient-as-coordinator is a stopgap, not a solution. Policy intervention required.
Ankit Right-hand for this but 2 qty HK 21
November 22, 2025 AT 15:06What a joke. You think this list thing is going to fix the fact that the entire healthcare system is rigged? The real problem is that doctors are paid to prescribe, not to coordinate. The pharmaceutical companies own the EHRs. The pharmacists are just sales reps with white coats. And you? You’re just a walking ATM with a pulse.
They don’t want you healthy. They want you on meds forever. That’s why they won’t talk to each other. If they did, you’d get better. And then they’d lose money.
Bring your list? Yeah, right. I did. They threw it in the trash. Said "we have it on file." They didn’t. They never do.
And don’t even mention the "care coordinator." That’s a title for the guy who’s too lazy to call anyone. He just sends you a form to fill out. Again.
This isn’t about communication. It’s about control. And you? You’re just the mark.