Generic Drug Switching: What You Need to Know Before You Switch
When your pharmacy hands you a different pill with the same name but a cheaper price, that’s generic drug switching, the practice of replacing a brand-name medication with a chemically identical generic version. Also known as medication substitution, it’s used by insurers, pharmacies, and state programs to cut costs—sometimes without telling you. But just because the active ingredient is the same doesn’t mean your body reacts the same. Many people notice changes in how they feel, even when the FDA says generics are bioequivalent.
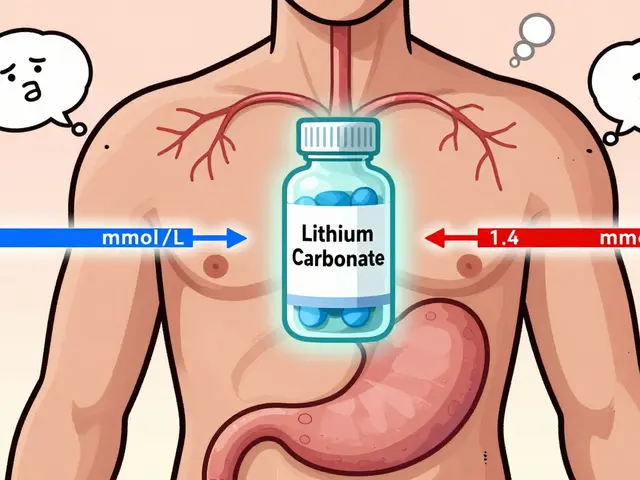
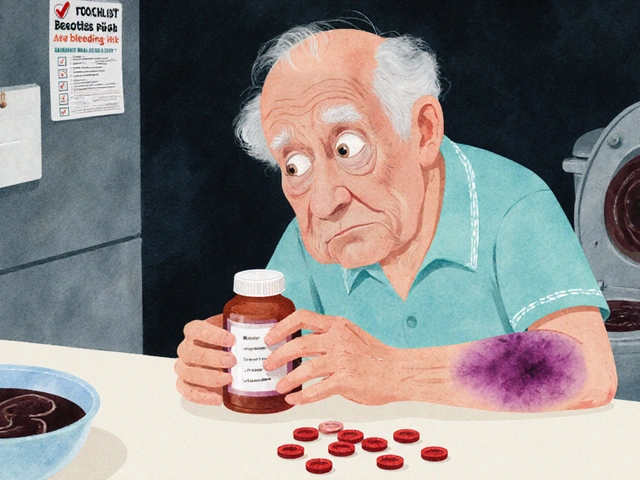
Brand-name drugs, the original versions developed by pharmaceutical companies often have patents that expire after 10–15 years. Once they do, other companies can make copies. These generic drugs, are required by law to contain the same active ingredient, strength, and dosage form. But fillers, dyes, and coatings? Those can vary. For most people, that’s fine. For others—like those on thyroid meds, seizure drugs, or blood thinners—it can mean the difference between control and crisis. One study found that 1 in 5 patients on warfarin had their INR levels shift after switching to a different generic version. That’s not rare. It’s routine.
Insurance plans push drug formulary, the list of medications they cover and at what cost changes to save money. If your plan puts a generic on Tier 1 (low copay) and the brand on Tier 3 (high copay), you’ll get the generic—even if your doctor didn’t prescribe it. Some states have laws that let pharmacists switch without asking. Others require consent. You might not know which one you live in. And if you’re on Medicaid, you’re even more likely to be switched, since 84.7% of prescriptions there are generics. But what happens when the generic runs out? That’s when generic drug shortages, caused by manufacturing failures and global supply chain gaps hit hard. You might get switched again—this time to a different generic, or worse, nothing at all.
It’s not about distrust. It’s about awareness. If you’ve ever felt off after a pill change—more tired, more anxious, less effective—that’s not in your head. It’s in the chemistry. And you have the right to ask why you were switched, to request your original brand, and to report any reaction to your pharmacist or the FDA. Below, you’ll find real stories and data on how insurance decides what you get, when switching works, when it doesn’t, and what to do if your body says no.

How to Choose Between Different Generic Medications for the Same Condition
Learn how to choose between different generic medications by understanding therapeutic equivalence ratings, bioequivalence standards, and when consistency matters most for your health.