Provider Communication: How to Talk to Doctors and Pharmacists About Your Medications
When you're taking multiple medications, provider communication, the clear, consistent exchange of information between patients and healthcare professionals about medications and treatment plans. Also known as medication coordination, it's not just polite—it’s life-saving. Too many people end up in the ER because their cardiologist doesn’t know what their rheumatologist prescribed, or their pharmacist didn’t get the updated list. This isn’t rare. Studies show over 50% of medication errors happen because of broken communication between providers.
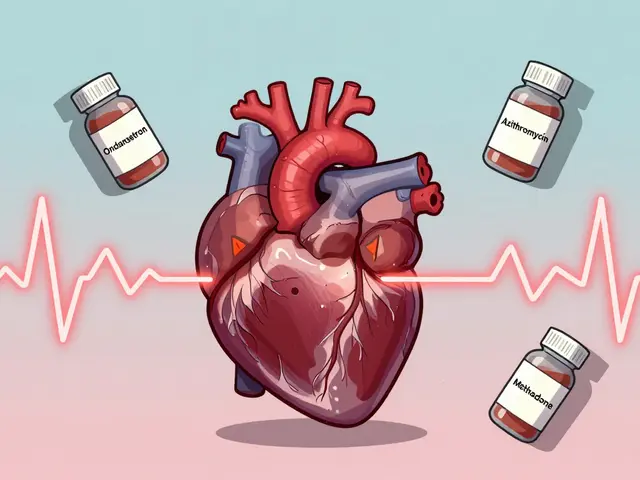
You don’t need to be a medical expert to fix this. You just need to be organized and speak up. Start with a simple medication list, a written or digital record of all drugs, doses, and reasons for use, including supplements and over-the-counter pills. Keep it updated. Carry it. Show it to every new provider—even if they say they can see your records. Most clinics still use paper charts or outdated systems. Your list is your backup. Then there’s the pharmacist, the most underused resource in your healthcare team, trained to catch drug interactions and dosing mistakes. Don’t just pick up your script. Ask: "Does this interact with my other meds?" or "Is there a cheaper version?" Pharmacists see hundreds of prescriptions a day. They’ll spot what your doctor might miss.
It’s not just about what you take—it’s about how you talk. If you’re seeing three doctors, who’s in charge? Who’s tracking everything? That’s your job to clarify. Say: "I’m seeing Dr. Lee for blood pressure and Dr. Patel for diabetes. Can you two coordinate?" Or better yet, ask your primary care doctor to be the hub. And if you’re on blood thinners, diabetes meds, or anything with a black box warning, don’t assume they know your full history. Bring your list. Ask questions. Write down answers.
This isn’t about being difficult. It’s about being smart. People who track their meds and ask clear questions have fewer hospital visits, fewer side effects, and better outcomes. The system isn’t perfect. But you can be the missing link.
Below, you’ll find real guides on how to handle complex medication situations—from managing multiple providers to spotting dangerous interactions, using barcode scanning systems, and even what to do when a drug suddenly disappears from shelves. These aren’t theory pieces. They’re tools made by people who’ve been in your shoes. Use them.

How to Report a Medication Error or Concern to Your Provider
Learn how to report a medication error to your provider or the FDA - step by step. Know your rights, the best reporting channels, and how your report can prevent harm to others.