BPH Medication Impact Calculator
How Medications Affect Your Intimacy
Choose your medication type to see potential impacts on sexual function and intimacy.
Results
Select your medication and concerns to see detailed results.
When a man receives a diagnosis of BPH benign prostatic hyperplasia, a non‑cancerous enlargement of the prostate that often brings urinary urgency, nighttime trips, and changes in sexual function, the impact stretches beyond the bathroom and into the bedroom.
Key Takeaways
- Understanding how BPH symptoms affect desire, performance, and emotional closeness helps couples tackle problems together.
- Open, non‑judgmental communication is the foundation for maintaining intimacy.
- Medications, lifestyle tweaks, and pelvic‑floor training can reduce symptoms without killing the spark.
- Professional support-urologists, therapists, or support groups-offers practical tools and reassurance.
- A simple checklist can keep you and your partner on the same page as you navigate changes.
What Is BPH and Why Does It Matter?
BPH affects about 50% of men over 60 and up to 90% by age85, according to recent urology surveys. The prostate sits beneath the bladder, encircling the urethra. When the gland swells, it squeezes the urethra, leading to the classic trio of symptoms: frequent urges, weak stream, and nocturnal trips. While the medical label sounds clinical, the lived reality often includes frustration, embarrassment, and a dip in confidence-feelings that seep into intimate moments.
Beyond the urinary side effects, many men notice a shift in erectile dysfunction the inability to achieve or maintain an erection sufficient for intercourse. Hormonal changes, nerve compression, and medication side‑effects all play a part, making the bedroom feel like a minefield.
How BPH Symptoms Ripple Into Intimacy
Intimacy isn’t just about sex; it’s the whole package of closeness, affection, and shared vulnerability. BPH can disrupt this in several ways:
- Physical interruptions - A sudden urge to dash to the bathroom mid‑moment creates awkward pauses.
- Self‑consciousness - Men may avoid sexual activity because they fear a weak stream or the need to urinate.
- Emotional disconnect - Repeated setbacks can usher in anxiety, depression, or resentment on both sides.
When one partner pulls back, the other may interpret it as rejection, deepening the divide. Recognising that the problem is physiological, not personal, is the first step toward rebuilding trust.
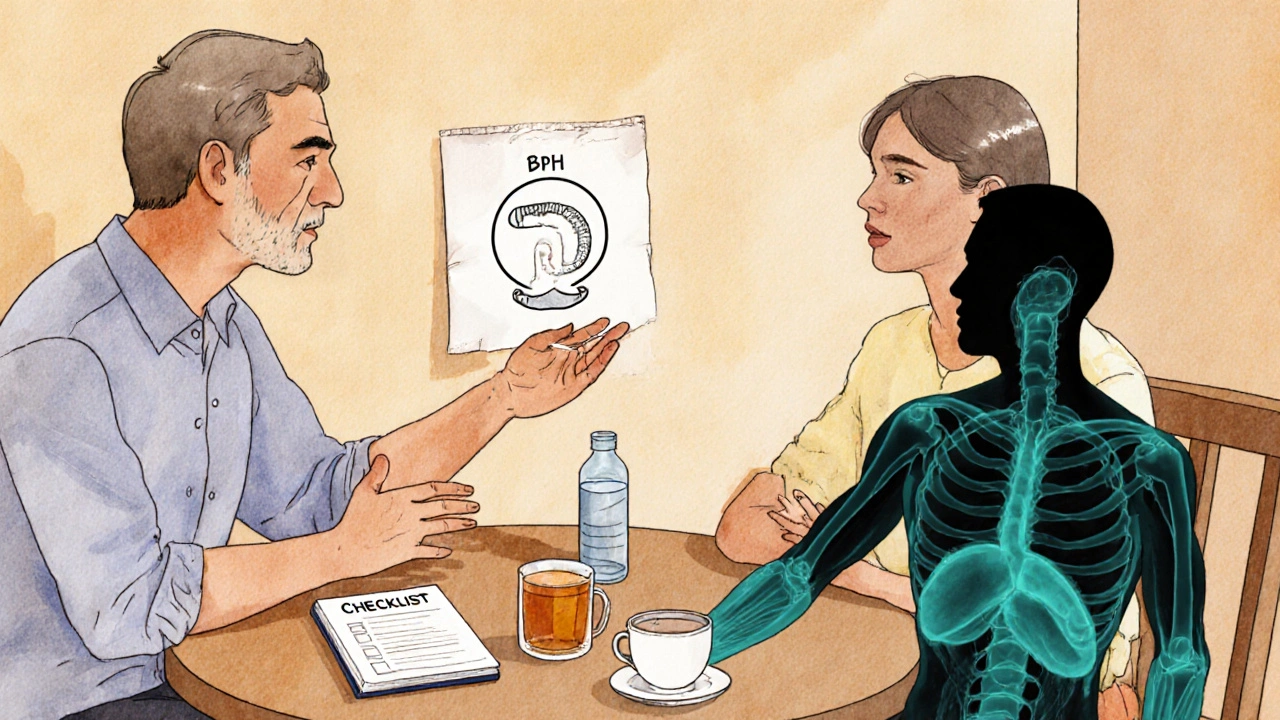
Talking About BPH With Your Partner
Transparent conversation can turn a source of shame into a joint problem‑solving mission. Here are practical tips that have helped real couples:
- Pick the right moment - Choose a calm, private setting, not right after a night‑time bathroom break.
- Use “I” statements - Phrase concerns as personal feelings (“I feel anxious when…”) rather than blame (“You never…”).
- Share the facts - Explain what BPH is, using simple analogies (e.g., “the prostate is like a ring that’s getting too tight”).
- Invite questions - Let your partner ask anything, even the embarrassing ones.
- Plan together - Discuss timing, bedroom accommodations (e.g., keeping a night‑lamp on), and any medication concerns.
When both sides feel heard, you can co‑create a roadmap that balances symptom management with affection.
Medical Options: What Works and What to Watch For
Urologists typically start with lifestyle tweaks, then prescribe medication if symptoms persist. Below is a quick comparison of the most common drug classes.
| Medication Type | Example Drugs | How It Works | Typical Side Effects | Impact on Sexual Function |
|---|---|---|---|---|
| Alpha‑blocker | Tamsulosin, Alfuzosin | Relaxes smooth muscle in prostate and bladder neck | Dizziness, low blood pressure | Generally neutral; occasional retrograde ejaculation |
| 5‑alpha‑reductase inhibitor | Finasteride, Dutasteride | Shrinks prostate by blocking DHT hormone | Decreased libido, erectile issues | May worsen erectile function initially, improves over months |
| Combination therapy | Tamsulosin + Finasteride | Targets both muscle tone and size | Combined side‑effect profile | Higher chance of sexual side effects; monitor closely |
Discuss any concerns with your doctor-especially if you’re already on medication for blood pressure or depression, as interactions can occur.
Lifestyle Tweaks That Lighten the Load
Simple daily habits can shave minutes off bathroom trips and keep the bedroom vibe alive.
- Fluid timing - Limit caffeine and alcohol after dinner; sip water steadily throughout the day instead of gulping right before bed.
- Dietary choices - Foods rich in zinc (pumpkin seeds, shellfish) and antioxidants support prostate health.
- Pelvic floor exercise - Strengthening the muscles that control urination can also improve erection quality. Pelvic floor exercise targeted contractions known as Kegels that boost urinary control and sexual stamina.
- Weight management - Excess body fat raises estrogen levels, which can aggravate BPH.
- Stress reduction - Mind‑body practices (yoga, deep breathing) lower cortisol, a hormone that can heighten urinary urgency.
Small wins add up: a couple who schedules a “no‑bathroom” half‑hour after dinner often reports a more relaxed evening.
When Emotions Take Over: Getting Professional Help
Even with meds and lifestyle changes, the emotional toll can linger. A therapist who specialises in sexual health or a men’s support group can provide tools like:
- Cognitive reframing - Replacing “I’m broken” with “I’m managing a health condition” reduces anxiety.
- Intimacy exercises - Non‑sexual touch, eye‑gazing, or shared hobbies rebuild closeness.
- Sexual counseling - A certified sex therapist can suggest positions, timing, or lubricants that accommodate reduced stamina.
Remember: seeking help is a sign of strength, not weakness. Many couples emerge more resilient after confronting the issue together.
Real‑World Example: Mike and Sarah’s Journey
Mike, 62, started noticing nighttime trips after dinner. He felt embarrassed and stopped initiating intimacy. Instead of keeping it to himself, he told Sarah, “I’m dealing with something that’s making me run to the bathroom a lot, and I’m scared it’s affecting us.” Sarah responded with empathy, and together they tried three changes: a) switching to tamsulosin, b) setting a “light‑break” rule (no heavy fluids after 8pm), and c) practicing Kegels daily. Within two months, bathroom trips dropped from six to two nightly, and they rediscovered a playful mood in the bedroom. Their story shows how a blend of medical, practical, and emotional steps works.
Checklist for Couples Facing BPH
- Schedule a urology appointment; write down symptoms and questions.
- Discuss BPH openly with your partner; use “I feel…” language.
- Choose a medication plan; note any sexual side‑effects.
- Implement fluid timing and diet adjustments.
- Begin pelvic‑floor exercises - 5seconds hold, 10 repetitions, twice daily.
- Set a nightly routine that includes a low‑light bathroom path.
- Check in weekly with each other about comfort, fears, and successes.
- If anxiety persists, book a session with a therapist specialising in sexual health.
Cross‑checking this list every few weeks helps you stay proactive and prevents small problems from becoming big rifts.
Frequently Asked Questions
Can BPH medications make erectile dysfunction worse?
Some drugs, especially 5‑alpha‑reductase inhibitors, can lower libido or make erections less firm at first. The effect often improves after a few months, and many men find the urinary relief outweighs the temporary dip. Talk to your doctor about switching to an alpha‑blocker if sexual side‑effects become a deal‑breaker.
Are pelvic‑floor exercises safe for older men?
Yes. Kegel‑type exercises strengthen the muscles that control urination and can also improve erection rigidity. Start slowly-ten gentle squeezes, hold for three seconds, then release. Consistency beats intensity.
Should my partner avoid sexual activity while I’m on BPH meds?
No need to stop altogether. Some couples find that a short “cool‑down” period after medication helps manage bathroom urgency. Communication about timing and comfort is key.
How long does it take for medication to reduce symptoms?
Alpha‑blockers often start working within days to weeks, while 5‑alpha‑reductase inhibitors may need three to six months to noticeably shrink the prostate.
Is it normal to feel embarrassed discussing BPH with my partner?
Absolutely. Many men experience shame because BPH involves the reproductive system. Normalising the conversation-treating it like any other health issue-helps remove the stigma.







John Barton
October 13, 2025 AT 16:10Oh great, another guide telling us how to "manage intimacy" with BPH-because nothing says romance like a midnight bathroom sprint. The dramatics of "emotional disconnect" are almost as compelling as a soap opera climax, and I’m sure every couple has a "playbook" for it. If you wanted a thriller, you’d have written a novel, not a medical checklist.
Achint Patel
October 21, 2025 AT 02:50One might ponder whether the physiological constraints are merely a metaphor for the existential angst that pervades modern masculinity. Yet, the article artfully dissects the corporeal mechanisms without succumbing to hyperbole, maintaining a commendable balance between anecdote and empirical rigor. It invites the reader to contemplate the nature of desire as a function of both neurochemical flux and societal narrative. Though the tone remains informal, the grammatical precision ensures clarity amidst the philosophical drift.
Charlie Martin
October 28, 2025 AT 12:30The fluid timing tip is essentially common sense.
Harshal Sanghavi
November 4, 2025 AT 23:10Look, the toolbox you’ve been handed isn’t a death sentence-think of it as a DIY kit for the bedroom. Start with the low‑hanging fruit: schedule a “no‑caffeine after 7 p.m.” rule and give those Kegels a shot; you’ll be surprised how quickly the urgency fades. If a medication side‑effect pops up, treat it like a temporary glitch, not a permanent sabotage.
Duke Gavrilovic
November 12, 2025 AT 09:50Observing the article, one notes a harmonious blend of clinical data and cultural sensitivity-quite the diplomatic dance. While the tone swings between casual anecdotes and formal references, the underlying message remains universally applicable. It’s a reminder that health discourse can be both approachable and respectfully scholarly.
Abby VanSickle
November 19, 2025 AT 20:30I appreciate the thoroughness of the checklist; it provides a concrete framework for couples navigating this sensitive issue. Addressing both physiological symptoms and emotional ramifications demonstrates a holistic approach that is often lacking in medical literature. Moreover, the encouragement to seek professional guidance underscores the importance of interdisciplinary care. Your emphasis on empathetic communication is commendable.
chris macdaddy
November 27, 2025 AT 07:10Man, I think the article is spot on, but let me add sumthin – keep the bathroom light dim so you dont feel like you are in a stadium each night. Also, try drinkin more water early in the day, not right before bed – it really helps. Its not just about meds, its about lifestyle changes that you can actually control. Keep it up, you’ll see improvements faster then you think.
Moumita Bhaumik
December 4, 2025 AT 17:50Don’t be fooled by the glossy charts and “expert” recommendations; the pharmaceutical industry has a vested interest in keeping men dependent on these side‑effect laden pills. Their secret agenda is to monetize every nocturnal bathroom trip, turning a natural aging process into a lifelong subscription. Question every label, and consider natural alternatives before signing away your autonomy.
Sheila Hood
December 12, 2025 AT 04:30While the article offers solid advice, it’s worth noting that many of the suggested exercises can be performed without a pricey physiotherapist. A simple routine of three sets of five‑second holds twice daily yields noticeable results for most men. Consistency, rather than complexity, is the real driver of improvement.
Melissa Jansson
December 19, 2025 AT 15:10Wow, let’s pull the fire alarm on this whole “BPH‑centric intimacy manual.” First, the premise that urinary urgency directly sabotages sexual performance is a reductionist oversimplification that ignores the neuroendocrine cascade governing libido. Second, the article’s reliance on “alpha‑blocker” versus “5‑alpha‑reductase inhibitor” dichotomy is a classic false binary, as real‑world pharmacodynamics involve a spectrum of receptor affinity and downstream signaling pathways. Third, the suggested pelvic floor regiment is tossed in as a panacea without acknowledging the variance in neuromuscular plasticity among aging males. Fourth, the narrative’s claim that “communication is the foundation” is a platitude that masks the underlying power dynamics of gendered vulnerability. Fifth, the checklist’s linear progression implies a one‑size‑fits‑all protocol, disregarding comorbidities such. as metabolic syndrome that modulate drug metabolism. Sixth, the adoption of “night‑time lamp” strategies is reminiscent of low‑tech solutions that fail to address the root etiological factors, such as dihydrotestosterone flux. Seventh, the article’s casual tone belies a covert agenda to normalize pharmaceutical dependence under the guise of lifestyle optimization. Eighth, the reference to “stress reduction” as a cure‑all neglects the biopsychosocial model’s complexity, where cortisol interacts with autonomic tone in a feedback loop. Ninth, the piece omits any discussion of emerging pharmacogenomic profiling that could tailor therapy to individual allelic variants. Tenth, the emphasis on “non‑judgmental communication” subtly reinforces the stigma that men must conceal physiological decline. Eleventh, the assertion that “most men find relief outweighs temporary side‑effects” is an anecdotal generalization lacking rigorous meta‑analysis. Twelfth, the article’s omission of alternative modalities-such as phytotherapy, cryotherapy, or minimally invasive laser ablation-creates an incomplete therapeutic landscape. Thirteenth, the reliance on “urologist” as the sole gatekeeper disregards the multidisciplinary potential of sex therapists and pelvic health physiotherapists. Fourteenth, the language of “rebuilding closeness” masks the fact that intimacy is a negotiated construct, not a static endpoint. Finally, while the checklist is aesthetically pleasing, its practical utility collapses under the weight of real‑world variability, making it more of a decorative infographic than a functional roadmap. In short, readers should approach this guide with a healthy dose of skepticism and demand evidence‑based nuance before committing to its recommendations.