When patients leave the doctor’s office confused, or when nurses and doctors miscommunicate during shift changes, the result isn’t just frustration-it’s risk. Poor communication in healthcare contributes to 80% of preventable medical errors, according to The Joint Commission. Yet most hospitals still treat communication like an afterthought, not a core skill. That’s changing. Institutional generic education programs are now being built into hospitals, clinics, and medical schools across the U.S. to fix this broken system. These aren’t fluffy workshops. They’re structured, evidence-based training programs designed to teach clinicians how to talk-really talk-to patients, colleagues, and communities.
Why Communication Training Isn’t Optional Anymore
It’s easy to assume good communication happens naturally. But research shows it doesn’t. A 2018 analysis by the Agency for Healthcare Research and Quality found that communication failures directly lead to 15-20% of adverse patient outcomes. That means in every 10 serious medical errors, at least one could have been prevented with better talk.
Patients who feel heard are less likely to sue. Physicians who complete communication training see up to a 30% drop in malpractice claims, according to a Johns Hopkins Medicine study. Hospitals with strong communication programs report higher HCAHPS scores-those patient satisfaction ratings that now affect 30% of Medicare reimbursements. And it’s not just about being nice. It’s about safety, efficiency, and legal protection.
During the pandemic, the stakes got even clearer. CDC after-action reports showed that 40% of early outbreak delays were tied to poor internal or public communication. When people didn’t understand mask guidelines or vaccine risks, misinformation spread faster than the virus. That’s when institutions realized: communication isn’t soft skills. It’s public health infrastructure.
What These Programs Actually Teach
Not all communication training is the same. Some focus on patient interactions. Others train teams to speak the same language. A few even teach how to handle media during a crisis. Here’s what the most effective programs cover:
- Eliciting the patient’s story-not just symptoms, but fears, beliefs, and daily life. The Program for Excellence in Patient-Centered Communication (PEP) at the University of Maryland trains clinicians to pause after the first sentence and ask, “What’s been on your mind?”
- Responding with empathy-not saying “I understand,” but naming the emotion: “It sounds like you’re scared this might come back.”
- Setting boundaries-how to say no to unreasonable demands without burning out. Nurses who took Mayo Clinic’s course reported a 40% drop in burnout after learning how to manage emotional overload.
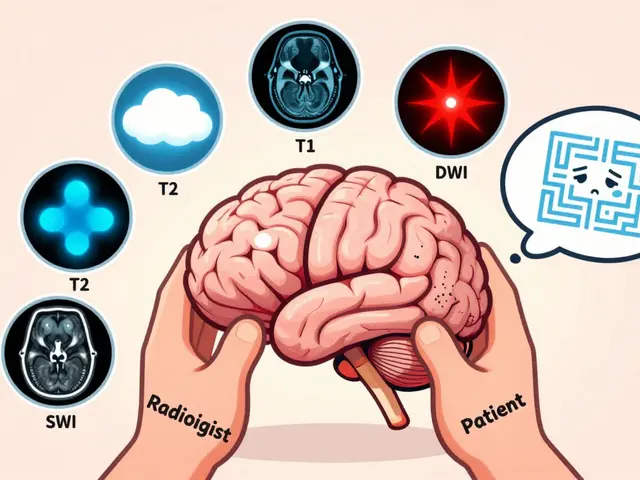
- Interprofessional communication-doctors, pharmacists, social workers all speak different jargon. Training teaches them to translate for each other.
- Public and policy communication-infection preventionists learn how to explain outbreaks to the press, not just to hospital staff.
These aren’t theoretical. They’re practiced. At Northwestern University, medical students go through 4-6 simulation sessions where they interact with trained actors playing patients with complex needs. They’re scored on specific behaviors. To pass, they must hit an 85% proficiency threshold. No exceptions.
How Programs Differ-and Who They’re For
There’s no one-size-fits-all. Different roles need different tools.
SHEA’s program (Society for Healthcare Epidemiology of America) targets infection control specialists. It’s a $75-$125 online course with modules on media relations and social media. One reviewer from Cleveland Clinic said it helped her correct vaccine misinformation reaching 50,000 people a month.
UT Austin’s HCTS focuses on public health emergencies. Their free pandemic communication course was updated in 2022 and now includes modules on health equity-because research shows minority patients report 28% lower satisfaction with communication than white patients.
Mayo Clinic’s course is for frontline staff. It uses 12 real patient videos to show how to handle angry families, cultural misunderstandings, and difficult conversations about end-of-life care. It’s accredited for nursing and social work credits.
Johns Hopkins’ Master’s in Communication is for those who want to lead. A 30-credit program costing $1,870 per credit, it’s designed for administrators, educators, and policy makers. But it’s not for someone who needs to fix communication tomorrow-it’s for someone who wants to change the system.

What Works-and What Doesn’t
Not all training sticks. A 2021 JAMA review found only 12% of programs track whether skills are used beyond six months. That’s the biggest failure.
Programs that work follow a clear model:
- Assess the gap-look at patient surveys, error reports, and staff feedback. What’s really breaking down?
- Pick 3-5 high-impact behaviors-don’t try to fix everything. Focus on what moves the needle.
- Teach in context-use real cases from your own clinic, not textbook examples.
- Embed it in workflow-add prompts to EHR systems. “Did you ask about concerns?” “Did you confirm understanding?”
Northwestern’s model-mastery learning-shows the best retention. After six months, learners kept 37% more skills than those who just sat through lectures. But it’s expensive. It needs simulation labs, trained actors, and time. Smaller clinics can’t afford that.
So what’s the alternative? Peer modeling. Mayo Clinic has senior physicians lead 60% of sessions. When a respected doctor says, “This changed how I talk to patients,” others listen.
The Real Barriers
Even the best program fails without support.
First, time. Doctors average just 13.3 seconds before interrupting a patient-even after training. In a 15-minute appointment, there’s no room for slow, careful talk.
Second, resistance. About 15-20% of clinicians believe communication can’t be taught. They say, “I’m just not good with people.” But studies show those same people improve after practice. It’s not talent-it’s technique.
Third, funding. Only 42% of hospital programs have dedicated budgets. Most rely on grants or one-time training dollars. Without ongoing support, skills fade.
And fourth, equity. Sixty percent of programs still don’t address cultural humility. Training a doctor to listen better means nothing if they don’t understand the patient’s background, language, or beliefs.
What’s Next
The field is evolving fast. In 2024, the Academy of Communication in Healthcare launched AI-powered feedback tools. Trainees record themselves, and the AI gives instant feedback on tone, pacing, and empathy cues. Pilot data shows 22% faster learning.
Telehealth is changing communication too. New programs now include virtual communication modules-how to read body language on Zoom, how to build trust without physical presence.
And the biggest shift? The National Academy of Medicine now calls communication a core healthcare function-like blood pressure monitoring or handwashing. That could mean mandatory training for all clinicians, not just optional courses.
Right now, 68% of large hospitals have formal programs. But only 22% of rural clinics do. The gap isn’t just about money-it’s about access. If communication training is the future of safe care, then everyone needs it.
Where to Start
If you’re a clinician wondering where to begin:
- Start small. Pick one skill: ask open-ended questions.
- Use free resources. UT Austin’s HCTS courses are free and include pandemic and equity modules.
- Ask your hospital if they have a communication program. If not, suggest starting with PEP’s open-access tools.
- Track your own results. Did fewer patients ask the same question twice? Did your team stop arguing during handoffs?
If you’re an administrator:
- Don’t buy a program off the shelf. Assess your own gaps first.
- Find champions-someone respected who’ll model the behavior.
- Link training to existing metrics: HCAHPS scores, error reports, turnover rates.
- Build in follow-up. One-hour training won’t change culture. Monthly check-ins will.
Communication isn’t about being charming. It’s about being clear, consistent, and human. And when done right, it saves lives-not just through better care, but by making sure the care that’s given is understood, trusted, and followed.
Are healthcare communication programs only for doctors?
No. These programs are designed for all healthcare staff-nurses, pharmacists, social workers, infection control specialists, and even administrative staff who interact with patients. Programs like SHEA’s target infection preventionists, while Mayo Clinic’s training is used by nurses and physician assistants. Communication is a team skill, not just a doctor’s responsibility.
How long does it take to see results from communication training?
Skill improvement can be seen within weeks-especially in patient satisfaction scores and team conflicts. But full integration into daily practice takes 3-6 months. Without ongoing reinforcement, skills decline. Programs that include follow-up sessions, EHR prompts, and peer coaching see the most lasting change.
Can communication training reduce medical errors?
Yes. Studies show communication failures cause up to 80% of preventable medical errors. Training that focuses on clarity, confirmation of understanding, and team handoffs reduces miscommunication during transitions of care-like when a patient moves from ER to floor or from hospital to home. Hospitals with structured programs report fewer medication errors and fewer missed diagnoses due to unclear reporting.
Are these programs covered by insurance or employer funding?
Many large hospitals and health systems cover the cost of training as part of staff development. Some programs, like UT Austin’s HCTS, are free. Others, like Mayo Clinic’s CNE course, offer credits that count toward licensure renewal. Employers benefit financially too-lower malpractice claims and higher HCAHPS scores can increase Medicare reimbursements by tens of thousands of dollars per year.
Do these programs address language and cultural barriers?
Increasingly, yes. In 2023, 74% of new programs included cultural humility training. But older or smaller programs often still lack this focus. Look for programs that specifically mention health equity, interpreter use, or bias awareness. UT Austin and Johns Hopkins now include modules on communicating with non-English speakers and addressing systemic disparities.
Is online training as effective as in-person simulation?
For basic knowledge, yes. Online courses are great for learning concepts and frameworks. But for skill mastery-like delivering bad news or managing an angry family-simulation with actors is far more effective. Northwestern’s data shows mastery learning leads to 37% higher retention. Online tools are improving with AI feedback, but they still can’t fully replace real human interaction in training.