Oxymetazoline Safety Checker
Oxymetazoline Hydrochloride is a topical nasal decongestant that works by narrowing blood vessels in the nasal passages, providing rapid relief from congestion caused by colds, allergies, or sinus inflammation. It is most commonly found in over‑the‑counter (OTC) nasal sprays and is approved for short‑term use (usually no more than three days) to avoid rebound congestion.
Why a Conversation with Your Doctor Matters
Even though oxymetazoline hydrochloride is sold without a prescription, speaking to a healthcare professional can prevent complications. Doctors can spot hidden risk factors like hypertension, thyroid disorders, or drug interactions that make the spray unsafe. They also help you understand when to stop using the product and what alternatives are better for chronic conditions such as allergic rhinitis.
Preparing for the Appointment
- Write down the exact product name, concentration (usually 0.05%), and how often you use it.
- Make a list of all current medications, including supplements and herbal remedies.
- Note any medical conditions you have - especially high blood pressure, heart disease, glaucoma, or diabetes.
- Bring a brief symptom diary showing when congestion starts, how long it lasts, and any side effects you notice.
Having this information ready makes the visit efficient and signals that you’re taking your health seriously.
Key Facts Your Doctor Will Want to Know
Below are the most common data points doctors ask about when you mention a nasal decongestant.
- Dosage
- Typical adult dosage: 1-2 sprays per nostril every 4-6 hours, not exceeding 2 sprays per nostril in a 24‑hour period (approximately 0.1mL per spray).
- Maximum Duration
- Use no longer than three consecutive days. Extending past this window increases the risk of rebound congestion, also known as rhinitis medicamentosa.
- Contraindications
- Patients with uncontrolled hypertension, severe coronary artery disease, or narrow‑angle glaucoma should avoid the spray unless cleared by a physician.
- Common Side Effects
- Temporary nasal dryness, stinging, or a mild bitter taste. Rarely, users experience headache, increased blood pressure, or tachycardia.
- Drug Interactions
- Concurrent use of monoamine oxidase inhibitors (MAOIs) or sympathomimetic drugs (e.g., pseudoephedrine) can amplify vasoconstrictive effects, leading to elevated blood pressure.
How to Phrase Your Concerns
Doctors appreciate clear, concise language. Try these starter sentences:
- "I’ve been using an oxymetazoline nasal spray for a week, and I’m still feeling congested after the third day. Should I stop?"
- "I have a history of hypertension. Is it safe for me to keep using this decongestant?"
- "I’m also taking pseudoephedrine for my sinus infection. Could the combination raise my blood pressure?"
- "I’ve noticed a burning sensation in my nose after each spray. Does that indicate an allergic reaction?"
- "If I need relief beyond three days, what alternative treatments would you recommend?"
These prompts make it easy for the clinician to assess safety and suggest next steps.

Managing Rebound Congestion
If you’ve used the spray for longer than recommended and now experience persistent blockage, you may be dealing with rhinitis medicamentosa. Here’s a simple plan:
- Gradual Weaning: Switch to a saline nasal spray for two days, then reduce oxymetazoline use by half each day.
- Topical Steroids: A short course of intranasal corticosteroids (e.g., fluticasone) can reduce inflammation and break the cycle.
- Hydration: Drink plenty of fluids and use a humidifier to keep nasal passages moist.
Always discuss weaning strategies with your doctor to avoid abrupt withdrawal that can worsen symptoms.
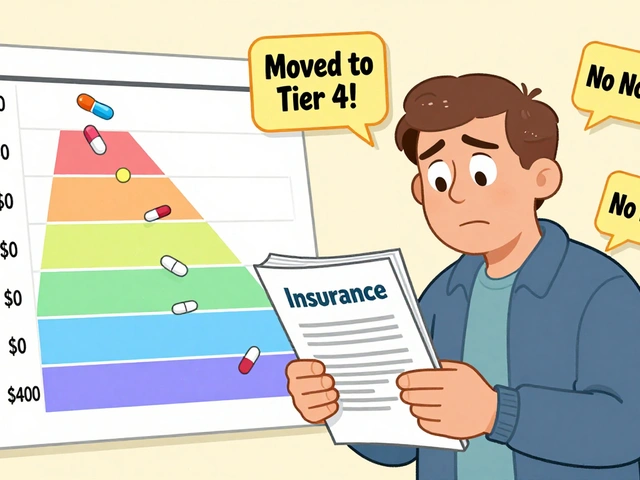
Alternatives - A Quick Comparison
| Product | Active Ingredient | Typical Duration of Safe Use | OTC Availability | Risk of Rebound |
|---|---|---|---|---|
| Oxymetazoline Spray | Oxymetazoline Hydrochloride | ≤3days | Yes | High if >3days |
| Phenylephrine Spray | Phenylephrine HCl | ≤3days | Yes | Moderate |
| Saline Nasal Spray | Isotonic NaCl solution | Unlimited | Yes | None |
Saline spray offers moisture without vasoconstriction, making it ideal for long‑term use or as a bridge while you wean off oxymetazoline.
Follow‑Up and Monitoring
After your appointment, keep an eye on the following indicators:
- Blood pressure readings (if you have hypertension, check twice daily for a week).
- Any new headaches or palpitations.
- Persistence of nasal blockage beyond three days.
If any of these symptoms appear, schedule a follow‑up within 48hours. Your doctor may order a basic metabolic panel to rule out systemic effects.
Related Concepts and Next Topics to Explore
Understanding oxymetazoline fits into a broader picture of nasal health. Consider diving deeper into these areas:
- Allergic Rhinitis - chronic inflammation caused by allergens, often managed with antihistamines and intranasal steroids.
- Sinusitis - infection or inflammation of the sinus cavities, sometimes requiring antibiotics or endoscopic surgery.
- Nasal Irrigation - a low‑cost, evidence‑based method to clear mucus and allergens using a neti pot or squeeze bottle.
- Intranasal Corticosteroids - first‑line therapy for persistent congestion, safe for long‑term use under medical supervision.
Each of these topics expands your toolbox beyond a single decongestant, helping you keep your nasal passages clear without reliance on short‑acting sprays.
Frequently Asked Questions
Can I use oxymetazoline if I have high blood pressure?
Only under a doctor’s guidance. The vasoconstrictive effect can raise systolic pressure by up to 5‑10mmHg, which may be risky for uncontrolled hypertension. Your physician might suggest a lower‑dose alternative or a non‑vasoconstrictive option like saline spray.
What should I do if I experience a burning sensation after each spray?
A mild burning feeling is common, but persistent or severe irritation could signal an allergic reaction or mucosal damage. Stop using the spray, rinse the nostrils with sterile saline, and call your doctor to discuss whether a gentler formulation or an alternative therapy is needed.
Is it safe to combine oxymetazoline with oral decongestants like pseudoephedrine?
Combining two sympathomimetic agents can amplify vasoconstriction, increasing the chance of hypertension, heart palpitations, or anxiety. Doctors usually advise against simultaneous use unless they closely monitor your vital signs.
How long does rebound congestion typically last?
If the underlying cause (over‑use) is addressed, symptoms often improve within 2‑5days after cessation. Adding a short course of intranasal steroids can speed recovery. Persistent blockage beyond a week warrants a follow‑up.
Can children use oxymetazoline nasal spray?
Most formulations are approved for children aged six and older, but dosage is halved compared to adults. For younger kids, physicians prefer saline irrigation or pediatric‑specific steroid sprays to avoid potential side effects.
What’s the difference between oxymetazoline and phenylephrine?
Both are α‑adrenergic agonists, but oxymetazoline has a slightly longer half‑life, providing up to 12‑hour relief per dose, whereas phenylephrine lasts about 4‑6hours. Oxymetazoline also carries a higher rebound‑congestion risk if overused.
Should I stop using the spray if I’m pregnant?
Pregnant women should avoid oxymetazoline unless a doctor deems it essential. Limited safety data exist, and the vasoconstrictive effect could affect fetal circulation. Safer options include saline sprays or physician‑prescribed steroid nasal sprays.





Rohan Puri
September 23, 2025 AT 17:21why are we even talking about this like it's a big deal i just use the spray when my nose is stuffed and stop when it's not why does everyone need a doctor for everything
Tracy McKee
September 25, 2025 AT 06:28people dont realize oxymetazoline is basically nasal crack you think you just need one more spray but its a trap the pharmaceutical companies know this and theyre fine with it because youll keep buying
Nicole Manlapaz
September 26, 2025 AT 02:07thank you for writing this so clearly i used to just blast the spray every time i felt stuffy until i got rebound congestion and it was awful this guide saved me
saline spray + humidifier + patience actually works
Frederick Staal
September 27, 2025 AT 06:34the fact that this is even a topic of discussion reveals the complete collapse of personal responsibility in modern healthcare
youre told to see a doctor for a nasal spray but youll go to a specialist for a headache caused by your own poor choices
the system is designed to make you dependent not healthy
Lee Lach
September 28, 2025 AT 12:22Let me offer a systems-level analysis of this phenomenon. Oxymetazoline hydrochloride is not merely a decongestant-it is a bioeconomic lever deployed by the pharmaceutical-industrial complex to cultivate chronic dependency under the guise of symptomatic relief. The three-day limit is not a safety feature-it is a regulatory fiction designed to allow for continuous repurchase cycles while avoiding liability. The FDA's approval of OTC status was a calculated concession to consumer autonomy, masking the reality that the drug’s pharmacokinetics are engineered to produce rebound rhinitis at precisely the point where consumer compliance begins to wane. This is not medicine. It is behavioral conditioning disguised as pharmacology. The alternatives listed-saline, steroids, irrigation-are not just options; they are acts of resistance against a system that profits from your nasal mucosa’s betrayal.
Kelley Akers
September 30, 2025 AT 07:52how is this even a post? anyone who needs a guide to using a nasal spray probably shouldn’t be allowed to buy it
like if you need a 2000 word manual to not overdose on a decongestant maybe you’re the problem not the product
erin orina
September 30, 2025 AT 09:34thank you for this! i’ve been using this for months and didn’t realize i had rebound congestion 😭
started saline spray last week and already feel better
you’re not alone if you’re stuck in this cycle 💙
Chris Bellante
October 1, 2025 AT 22:32in my clinic we see this every week. patients come in with chronic congestion from overusing sprays then blame the weather or allergies
the truth is simple: if you’re still using it after day three you’re not treating congestion you’re treating withdrawal
saline is your friend and so is your doctor
Abigail M. Bautista
October 2, 2025 AT 05:21why do we need all this info just to use a spray i just blow my nose and move on
Lisa Uhlyarik
October 3, 2025 AT 06:42you people are so naive oxymetazoline is just the tip of the iceberg
the real issue is that your body is being slowly poisoned by corporate chemicals and no one talks about it
the government knows but they let it happen because they’re paid off
saline spray won’t fix your soul
Mandeep Singh
October 3, 2025 AT 17:54why are americans so obsessed with doctors for everything in india we just use salt water and move on this is why your healthcare costs are insane