When you take an antibiotic for a sore throat or a sinus infection, you expect to feel better. But for some people, the very drug meant to help triggers something far worse: relentless diarrhea, cramps, and fever. This isn’t just a stomach upset. It’s Clostridioides difficile - a dangerous gut infection that’s become one of the most common hospital-acquired infections in the U.S. and a growing threat in the community.
What Exactly Is Clostridioides difficile?
Clostridioides difficile, often called C. diff, is a bacteria that lives quietly in the gut of about 5% of healthy adults. Normally, it’s kept in check by the trillions of good bacteria that make up your microbiome. But when antibiotics wipe out those helpful microbes, C. diff can take over. It doesn’t just multiply - it releases two powerful toxins that attack the lining of your colon. That’s when diarrhea, pain, and inflammation start.
It’s not new. Doctors first noticed the link between antibiotics and severe diarrhea in the 1950s. But it wasn’t until the 1970s, after a major outbreak tied to clindamycin, that scientists identified the culprit. Today, C. diff causes nearly half a million infections in the U.S. every year, according to the CDC. And it’s not just hospitals anymore - about 40% of cases now happen outside healthcare settings, in people who haven’t been hospitalized in the past year.
How Do You Get It?
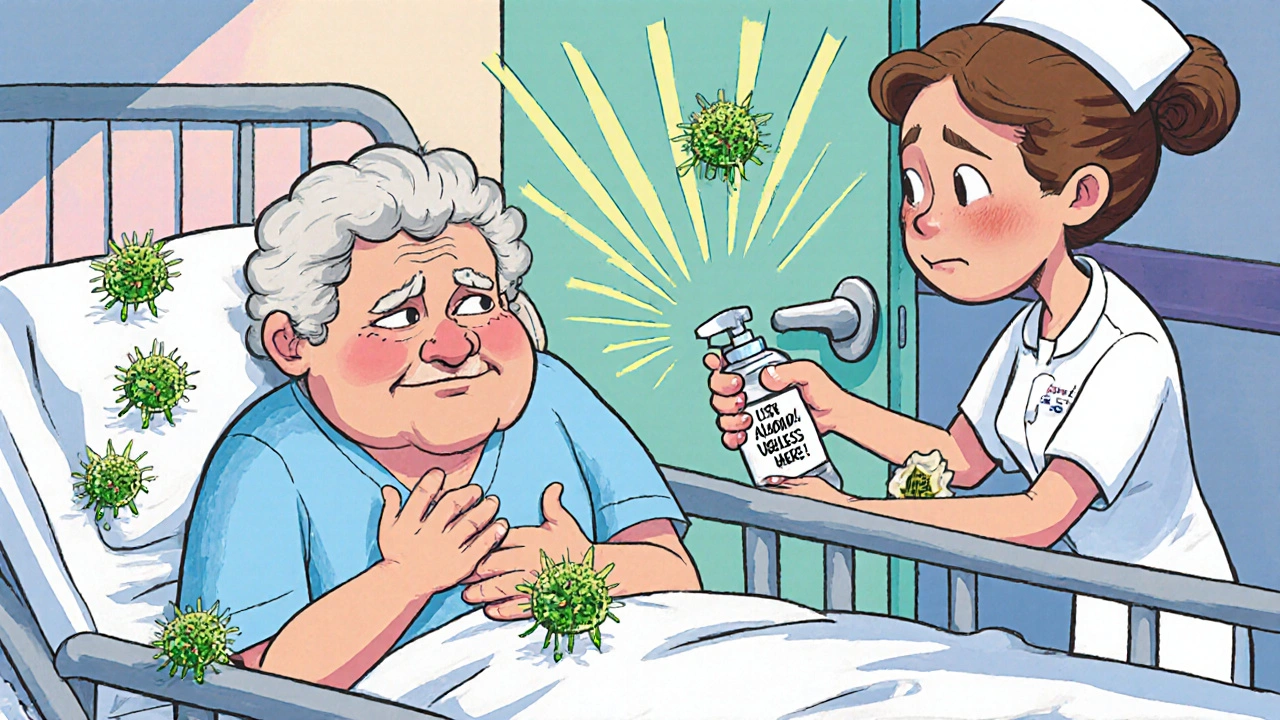
C. diff spreads through spores - tough, invisible shells that can survive for months on doorknobs, bed rails, toilets, and even clothing. You don’t need to be sick to carry them. Someone with C. diff can shed billions of spores in their stool. If you touch a contaminated surface and then touch your mouth, you can get infected.
But here’s the catch: most people who come into contact with C. diff spores never get sick. The real trigger? Antibiotics. Any antibiotic can do it, but some are worse offenders. Fluoroquinolones like ciprofloxacin, cephalosporins like ceftriaxone, clindamycin, and carbapenems are the biggest culprits. The longer you’re on them, the higher your risk. Each extra day in the hospital increases your chance of infection by about 1.5%.
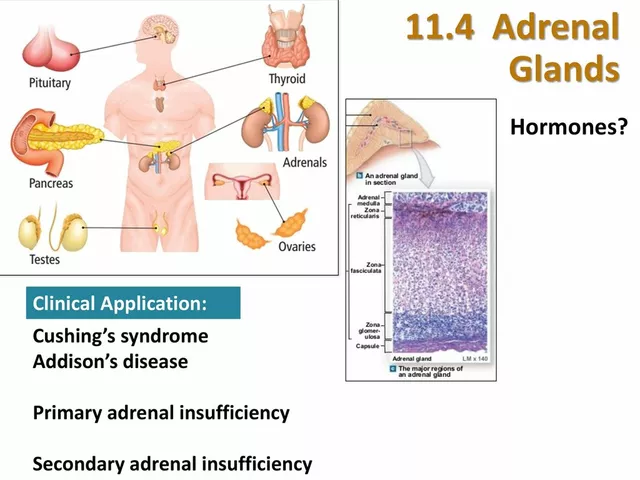
Age matters too. People over 65 make up 80% of all cases. Their immune systems are weaker, their gut microbiomes less resilient, and they’re more likely to be on multiple medications. People with inflammatory bowel disease (IBD) are 4 times more likely to get C. diff. So are those who’ve had recent gut surgery or are on acid-reducing drugs like proton pump inhibitors.
What Does C. diff Feel Like?
Symptoms can start as early as the first day of antibiotics - or as late as two months after you’ve finished them. That delay makes it easy to miss. Many people think it’s just a side effect of the meds, or food poisoning.
Early signs include:
- Loose, watery stools three or more times a day
- Abdominal cramping or pain
- Mild fever
- Loss of appetite
As it gets worse, you might see blood or pus in your stool. Your belly swells. You feel dizzy, your heart races, and your white blood cell count spikes. In severe cases, the colon can swell dangerously (toxic megacolon) or even rupture - a life-threatening emergency.
But here’s the tricky part: not everyone with C. diff in their gut has symptoms. Up to 50% of hospitalized patients carry the bacteria without being sick. That’s why testing alone isn’t enough. Doctors have to match lab results with your symptoms. If you’re not having diarrhea, you’re probably not infected - you’re just colonized.
How Is It Diagnosed?
Testing for C. diff isn’t straightforward. No single test is perfect. The CDC recommends a two-step process: first, a screening test for glutamate dehydrogenase (GDH), a protein the bacteria produce. If that’s positive, they follow up with a toxin test - either an enzyme immunoassay (EIA) or a nucleic acid amplification test (NAAT), which looks for the bacteria’s DNA.
Why two steps? Because NAATs are super sensitive - they’ll find even tiny amounts of C. diff DNA. But that means they can also pick up harmless colonization. Toxin tests, on the other hand, only detect active infection. Using both reduces false positives and false negatives. Alone, a single test can miss up to 30% of real infections.
And don’t assume your stool sample tells the whole story. If you’ve had diarrhea for less than 24 hours, or if you’re on certain medications, results can be misleading. Doctors rely on clinical judgment - your symptoms, your antibiotic history, your age - as much as the lab results.
How Is It Treated Now?
Treatment has changed dramatically in the last five years. Ten years ago, metronidazole was the go-to drug. Today? It’s no longer recommended as first-line therapy. Studies showed it’s less effective and leads to more recurrences.
Current guidelines from the Infectious Diseases Society of America (IDSA) and the American College of Gastroenterology say:
- For mild to moderate C. diff: fidaxomicin (200 mg twice daily for 10 days) is preferred. It’s more expensive, but it cuts recurrence rates in half compared to vancomycin.
- If fidaxomicin isn’t available: vancomycin (125 mg four times a day for 10 days) is the alternative.
- Never use metronidazole as a first choice anymore.
Fidaxomicin works differently. It kills C. diff without wiping out as many other gut bacteria. That’s why recurrence is lower - your microbiome has a better chance to bounce back.
For people who’ve had multiple recurrences - and about 20-30% of patients do - the best option is fecal microbiota transplantation (FMT). It’s not as wild as it sounds. Donors are carefully screened. Their stool is processed, filtered, and delivered via colonoscopy, capsule, or enema. Success rates? 85-90%. That’s far better than another round of antibiotics, which only works 40-60% of the time.
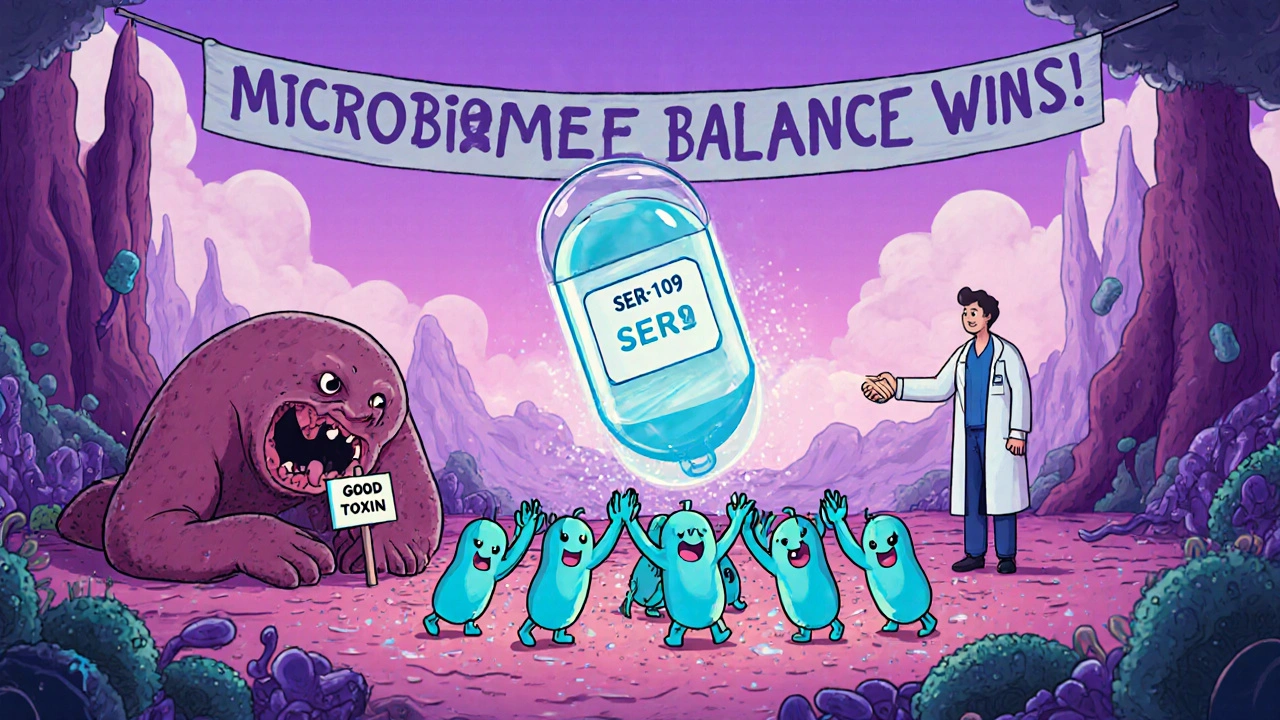
In 2023, the FDA approved the first microbiome-based drug for recurrent C. diff: SER-109. It’s a capsule filled with purified bacterial spores from healthy donors. In trials, it prevented recurrence in 88% of patients over 8 weeks. This is the future - targeted, precise, and microbiome-focused.
Can You Prevent It?
Yes - and the most powerful tool isn’t a drug. It’s restraint.
Antibiotic stewardship is the single most effective prevention strategy. Hospitals with strong stewardship programs have cut C. diff rates by 25-30%. That means:
- Only prescribing antibiotics when truly needed
- Choosing narrow-spectrum drugs over broad ones
- Shortening treatment duration when possible
- Avoiding antibiotics for viral infections like colds or flu
At home, ask your doctor: “Is this antibiotic really necessary?” If you’ve had C. diff before, be extra cautious. Don’t take antibiotics unless you’re sure they’re needed.
Environmental cleaning matters too. Regular hospital cleaners won’t kill C. diff spores. You need EPA-registered disinfectants from List K - those with bleach or hydrogen peroxide. If you’re visiting someone in the hospital, wash your hands with soap and water. Alcohol-based hand sanitizers don’t kill spores.
What about probiotics? Many people think yogurt or supplements can help. But the latest Cochrane review - analyzing nearly 10,000 patients - found no clear benefit for preventing C. diff. The American College of Gastroenterology explicitly advises against using them for this purpose. They might help with general antibiotic-related diarrhea, but not C. diff.
Why Is This Getting Worse?
One reason is the rise of hypervirulent strains, especially the NAP1/027 type. These bugs make more toxins, form more spores, and resist treatment better. They’re behind many of the severe outbreaks in hospitals and nursing homes.
Another reason? We’re still overusing antibiotics. In the U.S., about 30% of outpatient antibiotic prescriptions are unnecessary. That’s 47 million courses a year that could be avoided. Every unnecessary pill increases the risk - not just for you, but for everyone around you.
And while hospital infections have dropped 24% since 2011, community cases are rising. People who’ve never been hospitalized are getting sick. Why? Maybe it’s food, maybe it’s pets, maybe it’s environmental exposure. We’re still figuring it out.
What’s Next?
The future of C. diff management is about restoring balance, not just killing bacteria. Beyond FMT and SER-109, researchers are testing targeted antimicrobials, monoclonal antibodies to neutralize toxins, and even vaccines. Early trials look promising.
But until those become widely available, the best defense is simple: use antibiotics wisely, clean surfaces properly, wash your hands with soap, and know the signs. If you’re on antibiotics and develop diarrhea - especially if it’s watery, frequent, or lasts more than a couple of days - don’t brush it off. Talk to your doctor. Early diagnosis saves lives.
C. diff isn’t inevitable. It’s preventable. And it starts with asking the right questions - before you even pick up that prescription.




Stephen Adeyanju
November 26, 2025 AT 09:30Aaron Whong
November 26, 2025 AT 10:07Sanjay Menon
November 27, 2025 AT 10:27james thomas
November 28, 2025 AT 07:56Deborah Williams
November 28, 2025 AT 14:31Kaushik Das
November 29, 2025 AT 14:33Asia Roveda
November 29, 2025 AT 23:12Micaela Yarman
December 1, 2025 AT 21:30mohit passi
December 3, 2025 AT 06:24Marissa Coratti
December 4, 2025 AT 03:51Rachel Whip
December 6, 2025 AT 00:24Ezequiel adrian
December 7, 2025 AT 14:05