Medication Changes: What Happens When Your Prescription Shifts
When your medication changes, a shift in your prescription that can come from insurance rules, pharmacy substitutions, or doctor decisions. Also known as drug switching, it’s not just a paperwork update—it can affect how you feel, what you pay, and even your long-term health. Most people assume a generic pill is just a cheaper version of the brand name. But sometimes, that switch triggers new side effects, unexpected interactions, or even breaks your treatment plan. You might not realize it’s the medication change causing the problem—until you’re dizzy, nauseous, or your blood sugar spikes.
Behind every generic drug, a chemically identical version of a brand-name medicine approved by the FDA. Also known as brand equivalent, it is often the default choice for insurers and pharmacies is a complex system of insurance rules, manufacturing limits, and cost controls. insurance formularies, lists of drugs covered by a health plan, often with tiers that push patients toward cheaper options force you to try generics first—sometimes even after you’ve found a brand that works. And if your doctor doesn’t fight for an exception, you might end up on a different generic than last month, or worse, a different manufacturer entirely. Not all generics are made the same. Some have different fillers, coatings, or release rates that can change how your body absorbs the drug. That’s why people report new side effects after switching—even when the label says it’s the same.
Then there’s the hidden layer: drug interactions, when two or more medications affect each other’s effectiveness or safety. A change in your blood pressure med might clash with a supplement you started. A new antibiotic could mess with your birth control or thyroid pill. Even something as simple as switching from one antidepressant to another generic version can trigger anxiety, fatigue, or brain fog. And if you’re on multiple meds—say, for diabetes, heart disease, and depression—each change adds risk. One small switch can ripple through your whole system.
What you’re seeing in the posts below isn’t random. It’s the real-world fallout of these changes. You’ll find stories about people who got sick after a generic switch, others who fought insurance to keep their original drug, and guides on how to spot when a change isn’t safe. There’s advice on talking to your pharmacist, decoding your insurance formulary, and knowing when to push back. You’ll learn why some states have stronger protections than others, how manufacturing shortages force sudden switches, and what to do if your new pill doesn’t feel right. This isn’t about theory. It’s about what happens when your medicine changes—and how to take back control.
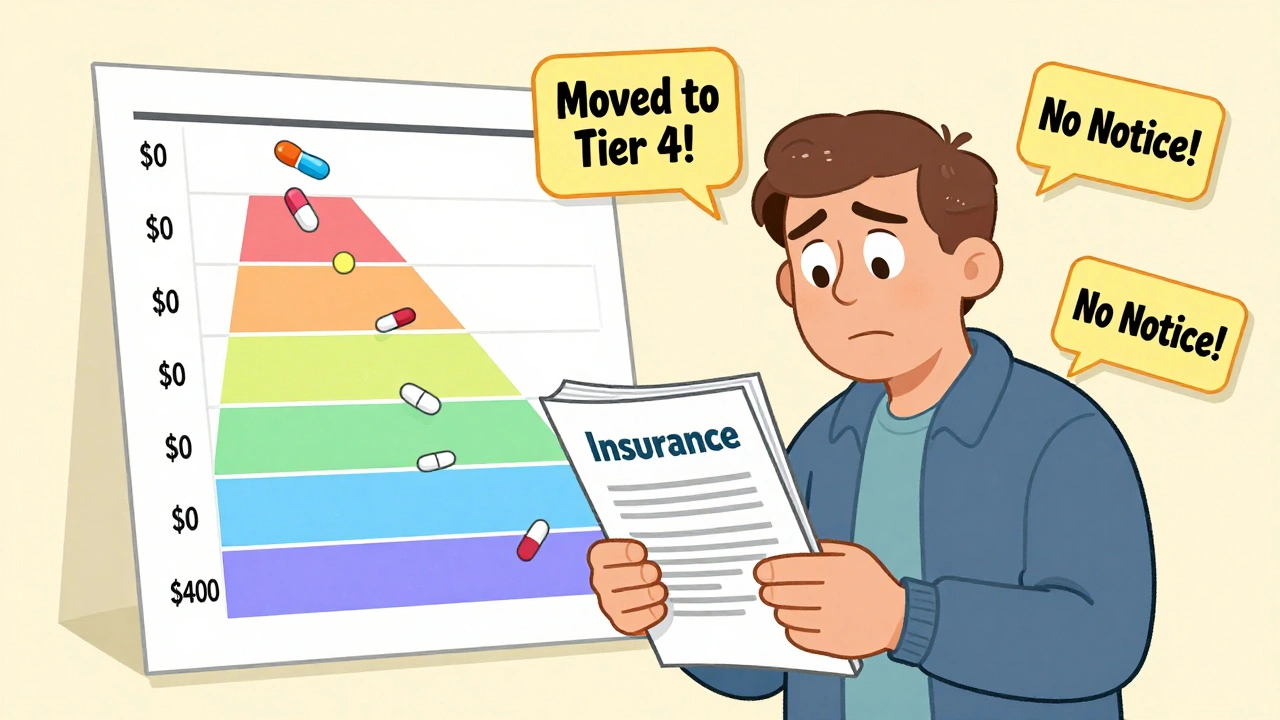
Insurance and Medication Changes: How to Navigate Formularies Safely in 2025
Learn how to navigate insurance formularies safely in 2025, avoid unexpected drug cost hikes, and ensure continuous access to your medications with step-by-step guidance and real-world tips.