API Manufacturing: What It Is, Why It Matters, and What You Need to Know
When you take a pill for high blood pressure, diabetes, or depression, the part that actually does the work is called the active pharmaceutical ingredient, the chemical compound responsible for the therapeutic effect in a medication. Also known as API, it’s the reason the drug works—everything else is just filler, coating, or stabilizer. But here’s the thing: API manufacturing isn’t just mixing powders in a lab. It’s a high-stakes, tightly controlled process that decides whether your medicine is safe, effective, or even legal.
Most of the world’s APIs are made in just a few countries, mostly India and China. These facilities must follow strict rules called GMP—Good Manufacturing Practices. But not all do. A single mistake in temperature, mixing time, or raw material purity can turn a life-saving drug into a dangerous one. That’s why quality assurance in manufacturing isn’t just a checkbox—it’s a survival tool, especially as drug prices drop and pressure to cut costs rises. You might not see the API, but you feel its impact: a pill that doesn’t work, a side effect that shouldn’t be there, or a recall that hits the news.
API manufacturing connects directly to the drugs you use every day. The generic drugs, lower-cost versions of brand-name medications that contain the same active ingredient you buy online or at the pharmacy? They rely on the same API as the brand name—but sometimes from a different factory, with different oversight. And that’s why some people notice differences in how a generic works compared to the original. It’s not always about the API itself, but how it’s made, purified, and blended. Even small variations can affect how fast your body absorbs it, which matters for drugs like blood thinners or seizure meds.
That’s also why pharmaceutical manufacturing, the full process of turning raw chemicals into finished, packaged medicines is under more scrutiny than ever. In 2025, quality failures cost more than ever—not just in dollars, but in lives. A single batch of contaminated API can trigger recalls across continents. That’s why barcode scanning in pharmacies, INR monitoring for blood thinners, and reporting medication errors all start with one thing: a reliable API. If the core ingredient isn’t pure and consistent, nothing else matters.
You won’t find API manufacturing listed on your prescription label. But if you’ve ever wondered why one generic works better than another, why your doctor switched your meds, or why some drugs get pulled from the market, the answer often starts in a factory thousands of miles away. The posts below dive into real cases—how bad manufacturing affects diabetes control, why some blood thinners need tighter monitoring, and how quality gaps can lead to hidden risks. These aren’t theory pieces. They’re real stories from people who’ve been affected. And they’ll help you ask the right questions before you fill your next prescription.

Supply Chain Problems: Distribution Risks for Generic Drugs
Generic drug shortages are at record levels due to overseas manufacturing, thin profit margins, and lack of backup suppliers. Learn why life-saving medications keep disappearing and what’s being done to fix it.
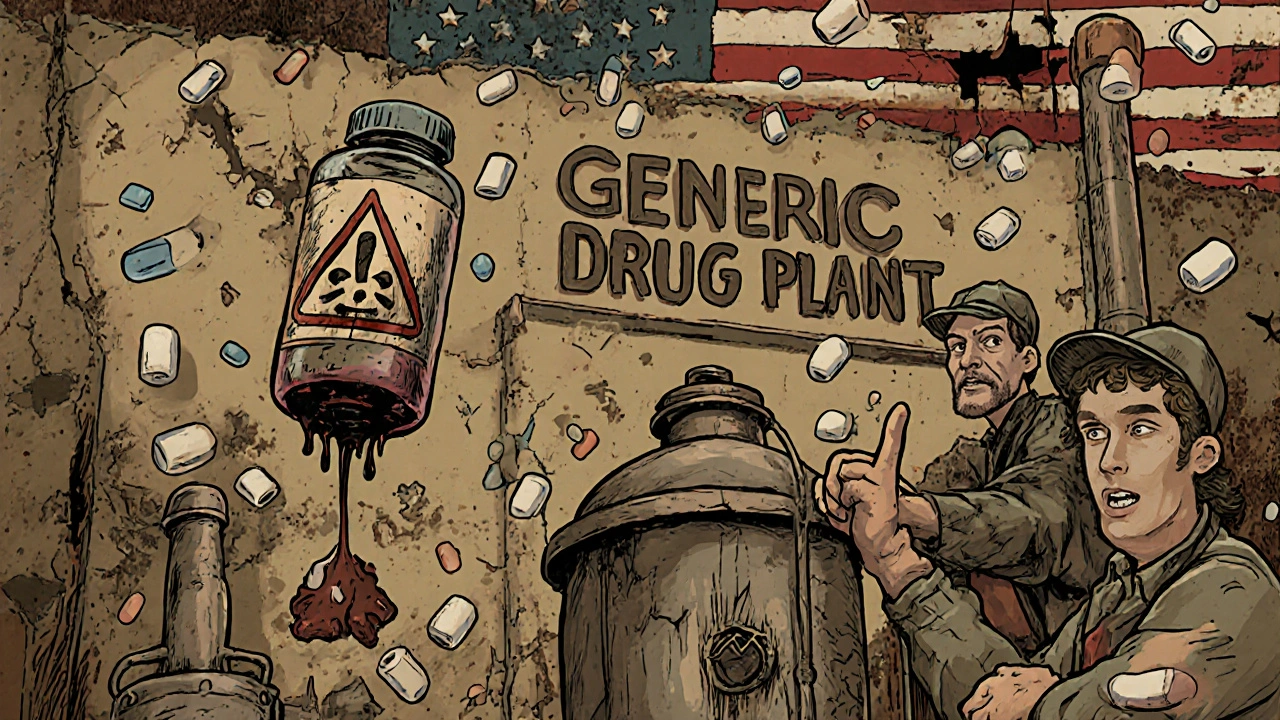
Causes of Generic Drug Shortages: Manufacturing and Supply Chain Issues
Generic drug shortages are caused by fragile manufacturing systems, global supply chain risks, and broken economics. Over 60% of shortages stem from production failures, with most active ingredients coming from just two countries. Low profits discourage investment, leaving no safety net when things go wrong.





