Hypertension Medication Comparison Tool
Dosing Frequency
Key Concerns
Special Considerations
If you’ve been prescribed Procardia (Nifedipine), you’re probably wondering how it stacks up against other blood‑pressure pills. This guide breaks down the science, side‑effects, and real‑world use cases so you can decide whether to stay put or consider a switch.
Key Takeaways
- Procardia is a short‑acting calcium‑channel blocker that works fast but may need multiple daily doses.
- Amlodipine offers once‑daily dosing with a smoother blood‑pressure curve, but can cause ankle swelling.
- ACE inhibitors like Lisinopril address the renin‑angiotensin system and are kidney‑friendly, yet cough is a common complaint.
- Losartan, an ARB, avoids the cough issue but may be less potent for severe hypertension.
- Non‑DHP calcium blockers (Diltiazem, Verapamil) also lower pressure but have stronger heart‑rate effects.
How Procardia Works
Procardia belongs to the dihydropyridine (DHP) class of Calcium channel blocker. It blocks L‑type calcium channels in the smooth muscle of arterial walls, preventing calcium influx that would otherwise cause contraction. The result is relaxed vessels and reduced peripheral resistance, lowering systolic and diastolic pressure.
When Doctors Prescribe Procardia
Typical indications include:
- Essential hypertension (especially when rapid control is needed).
- Chronic stable angina - the drug improves oxygen delivery by dilating coronary arteries.
- Hypertensive emergencies combined with IV therapy (rarely used alone).
Because Procardia acts quickly, it’s handy for patients who need short‑term pressure drops, such as pre‑surgical preparation.
Common Side Effects & Cautions
Most side effects stem from the vasodilatory action:
- Flushing and headache - the most frequent complaints.
- Peripheral edema - especially around ankles.
- Rapid heart rate (reflex tachycardia) - can be problematic for patients with arrhythmias.
- Gum hyperplasia - rare but reported with long‑term use.
Contra‑indications include severe aortic stenosis, uncontrolled heart failure, and known hypersensitivity to nifedipine.
Top Alternatives Overview
Below are the most widely used alternatives, grouped by drug class.
- Amlodipine - another DHP calcium‑channel blocker, but long‑acting. \n
- Lisinopril - an ACE inhibitor targeting the renin‑angiotensin‑aldosterone system.
- Losartan - an angiotensin‑II receptor blocker (ARB) with a similar profile to ACE inhibitors.
- Diltiazem - a non‑DHP calcium channel blocker with stronger heart‑rate slowing effects.
- Verapamil - another non‑DHP agent, often used for rate control in atrial fibrillation.
- Hydrochlorothiazide - a thiazide diuretic that reduces plasma volume.
- Metoprolol - a beta‑blocker useful for patients with concurrent heart‑rate issues.
Side‑by‑Side Comparison
| Drug | Class | Typical Dose | Frequency | Primary Use | Common Side Effects | Pros | Cons |
|---|---|---|---|---|---|---|---|
| Procardia (Nifedipine) | Dihydropyridine Ca‑channel blocker | 30‑60 mg | 2‑3 times daily | Hypertension, angina | Flushing, headache, edema, tachycardia | Fast onset, good for acute pressure drops | Multiple doses, reflex tachycardia |
| Amlodipine | Dihydropyridine Ca‑channel blocker | 5‑10 mg | Once daily | Hypertension, chronic angina | Peripheral edema, dizziness | Convenient dosing, stable BP control | May cause swelling, slower onset |
| Lisinopril | ACE inhibitor | 10‑40 mg | Once daily | Hypertension, heart failure | Cough, elevated potassium | Renal protection, good for diabetics | Dry cough, contraindicated in pregnancy |
| Losartan | Angiotensin‑II receptor blocker | 25‑100 mg | Once daily | Hypertension, nephropathy | Dizziness, hyperkalemia | No cough, kidney‑friendly | May be less potent for severe HTN |
| Diltiazem | Non‑DHP Ca‑channel blocker | 30‑180 mg | Once or twice daily | Hypertension, rate control | Constipation, bradycardia | Controls heart rate, useful in AF | Can depress cardiac contractility |
| Verapamil | Non‑DHP Ca‑channel blocker | 80‑240 mg | Once or twice daily | Hypertension, arrhythmias | Constipation, low BP | Strong anti‑arrhythmic effect | May worsen heart failure |
| Hydrochlorothiazide | Thiazide diuretic | 12.5‑25 mg | Once daily | Hypertension, edema | Electrolyte loss, photosensitivity | Effective low‑cost option | May increase uric acid, gout risk |

Choosing the Right Alternative
Consider these scenarios:
- Need for once‑daily dosing: Amlodipine, Lisinopril, Losartan, or a thiazide diuretic are better choices.
- Patient experiences chronic cough with ACE inhibitors: Switch to Losartan or a calcium‑channel blocker.
- Peripheral edema is intolerable: Diltiazem or Verapamil may cause less swelling but watch heart‑rate effects.
- Kidney disease: ARBs (Losartan) and ACE inhibitors (Lisinopril) provide renal protection, unlike most calcium blockers.
- Concurrent atrial fibrillation: Non‑DHP blockers (Diltiazem, Verapamil) help control rate while lowering BP.
Practical Tips for Switching or Combining
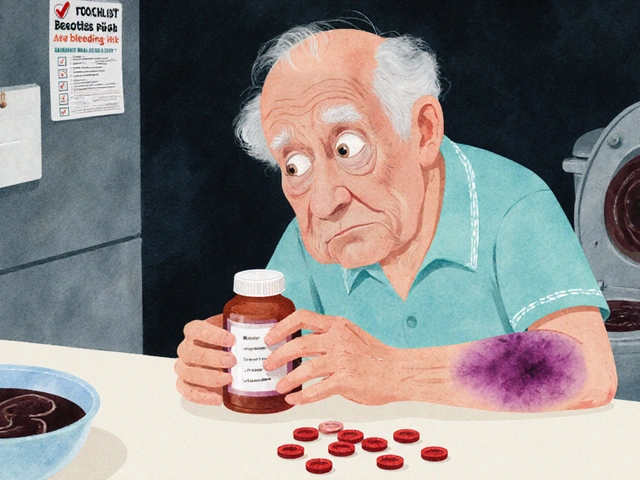
- Never stop Procardia abruptly; taper over 2‑3 days to avoid rebound hypertension.
- If moving to a long‑acting DHP like Amlodipine, start with a low dose (5 mg) and monitor BP for 1‑2 weeks.
- When adding a diuretic, watch for electrolyte shifts-check potassium and sodium after the first week.
- For patients on beta‑blockers, ensure heart rate remains above 50 bpm after any calcium‑blocker switch.
- Always review current drug‑interaction lists; nifedipine interacts with grapefruit juice, while ACE inhibitors interact with potassium‑rich salts.
Frequently Asked Questions
Can I take Procardia and Amlodipine together?
Combining two DHP calcium‑channel blockers offers no added benefit and heightens the risk of low blood pressure and swelling. Doctors usually switch, not stack.
What should I do if I develop a persistent cough on Lisinopril?
A dry cough is a classic ACE‑inhibitor side effect. Discuss with your clinician; they’ll likely switch you to an ARB like Losartan, which doesn’t cause cough.
Is Procardia safe during pregnancy?
Nifedipine falls into FDA Category C, meaning risk cannot be ruled out. It’s generally avoided unless the benefit outweighs potential harm.
Why does my ankle swell on Procardia but not on Amlodipine?
Both are DHP blockers, but Procardia’s shorter half‑life leads to more pronounced vasodilation spikes, which can trigger edema. Amlodipine provides steadier dilation, often reducing swelling.
Can I replace Procardia with a diuretic alone?
Diuretics lower blood pressure by reducing fluid volume, but they don’t relax arterial walls. For many patients, a combination of a diuretic and a calcium‑blocker works best. Solo diuretic therapy may be insufficient for severe hypertension.




ahmed ali
October 26, 2025 AT 21:20Alright, let me break this down for anyone still buying into the hype around Procardia.
First, the so‑called “fast onset” is a double‑ edged sword because those sudden drops can trigger reflex tachycardia that most patients can’t handle.
Second, the multiple daily dosing isn’t just an inconvenience; it creates peaks and troughs that defeat the whole purpose of steady blood‑pressure control.
Third, you’ll hear clinicians brag about “quick control,” but they forget that the body quickly compensates by releasing catecholamines, which actually raises the long‑term risk of cardiovascular events.
Fourth, the peripheral edema you get on Procardia isn’t a minor nuisance-it reflects fluid escaping into the interstitial space because of uneven vasodilation.
Fifth, the headache and flushing are not just side‑effects, they’re warning signs that the vascular smooth muscle is being overstimulated.
Sixth, the drug’s interaction with grapefruit juice isn’t a footnote; it can push plasma levels into a dangerous zone, a fact that many prescribing info sheets conveniently downplay.
Seventh, the short‑acting nature means you’re essentially playing “musical chairs” with your BP throughout the day, and that isn’t ideal for anyone with comorbid heart disease.
Eighth, if you’re on a beta‑blocker, the reflex tachycardia can nullify the protective effect of the beta‑blockade, leading to arrhythmic risk.
Ninth, the claim that Procardia is “kidney‑friendly” is misleading; the rapid shifts can actually stress renal perfusion in susceptible patients.
Tenth, the literature shows that patients switched to a long‑acting DHP like amlodipine have fewer emergency visits due to BP spikes.
Eleventh, the cost factor is rarely discussed, but the need for multiple pills a day adds up, especially when insurance plans favor once‑daily generics.
Twelfth, the “quick switch” protocols many doctors tout often ignore the 2‑3 day taper requirement, which can cause rebound hypertension.
Thirteenth, the alleged benefit for angina is marginal compared to beta‑blockers or nitrates that address myocardial oxygen demand more directly.
Fourteenth, the “real‑world use” data from pharmacy claims actually show higher discontinuation rates for Procardia than for amlodipine or lisinopril.
Fifteenth, if you’re looking for a stable, once‑daily regimen, the evidence points you toward a long‑acting agent, not this short‑acting roller coaster.
Sixteenth, so before you stay on Procardia, ask yourself if you really want a drug that feels like a daily juggling act rather than a set‑and‑forget solution.
Deanna Williamson
October 27, 2025 AT 01:30While the guide lists a slew of alternatives, it glosses over the fact that many clinicians avoid Procardia precisely because of inconsistent BP control.
The side‑effect profile isn’t just a checklist; the edema and headache often lead to poor adherence, which the article fails to emphasize.
Moreover, the comparison table omits cost considerations, which can be a decisive factor for patients on a fixed income.
The claim that Procardia’s fast onset is beneficial neglects the physiological stress of rapid vasodilation.
Overall, the piece skims the surface without addressing the real-world drawbacks that drive prescription changes.
Miracle Zona Ikhlas
October 27, 2025 AT 05:40Great rundown-thanks for laying everything out so clearly!
naoki doe
October 27, 2025 AT 09:50Honestly, if you’re juggling a 9‑to‑5 job and family duties, the multiple daily doses of Procardian can feel like a relentless reminder of your condition, whereas a once‑daily option lets you forget about pills until the next refill.
Joe Langner
October 27, 2025 AT 14:00Think of your blood pressure meds like a compass: Procardia points you quickly toward calm waters, but a steadier compass like amlodipine keeps you on course without the sudden gusses that shake the boat.
Even if you stumble over a few side‑effects, remember each hurdle is just a lesson teaching your body rehablence.
So, if you’re feeling uneasy, chat with your doc about a gentle transition-sometimes the journey matters more than the destination.
Katherine Brown
October 27, 2025 AT 18:10It is commendable that the author has presented a balanced overview of therapeutic alternatives; such comprehensive analyses are indispensable for clinicians seeking evidence‑based guidance.
Charlene Gabriel
October 27, 2025 AT 22:20When navigating the labyrinth of antihypertensive therapy, it helps to envision each class of medication as a distinct tool in a well‑stocked toolbox, each serving a specific purpose while complementing the others.
For patients who value simplicity, the once‑daily dosing schedule of amlodipine or an ARB like losartan can reduce pill fatigue and improve adherence, a factor that often translates into better long‑term outcomes.
Conversely, for those who require rapid titration or who are preparing for a surgical procedure, the quick‑acting nature of Procardia can provide the needed flexibility, provided that clinicians monitor for reflex tachycardia and edema.
It is also worth noting that calcium‑channel blockers, while effective, may exacerbate peripheral swelling, which can be particularly bothersome for individuals who already experience joint discomfort.
In contrast, ACE inhibitors such as lisinopril offer renal‑protective benefits, especially in diabetic patients, though the hallmark dry cough can be a deterrent for many.
Switching to an ARB like losartan often mitigates that cough while preserving the antihypertensive efficacy, making it a valuable alternative for cough‑sensitive individuals.
Moreover, the addition of a thiazide diuretic can enhance natriuresis, yet clinicians must remain vigilant about electrolyte disturbances, especially potassium and uric acid levels.
Beta‑blockers, exemplified by metoprolol, bring the advantage of heart‑rate control, which synergizes well with non‑DHP calcium blockers when managing patients with concomitant arrhythmias.
Ultimately, the choice of therapy should be individualized, taking into account comorbidities, lifestyle preferences, and the patient’s tolerance for side‑effects, rather than adhering rigidly to a one‑size‑fits‑all paradigm.
By fostering open dialogue and shared decision‑making, healthcare providers can empower patients to select the regimen that aligns best with their personal health goals and daily routines.
Leah Ackerson
October 28, 2025 AT 02:30Life is a series of choices, and the decision to cling to a drug that spikes your blood pressure like a roller coaster is, frankly, a philosophical misstep 😏.
If you prefer stability over drama, the literature subtly nudges you toward agents with smoother profiles, yet many still chase the fleeting thrill of rapid onset.
Remember, the path of least resistance often leads to the most sustainable health outcomes; embracing a once‑daily pill is a quiet act of wisdom 🌱.
Don’t let the allure of “quick fixes” blind you to the long‑term harmony that a steady regimen can provide.
Gary Campbell
October 28, 2025 AT 06:40What most people don’t realize is that the pharmaceutical lobby has a vested interest in keeping Procardia alive on the market because its multiple‑dose schedule inflates prescription counts, a fact hidden behind the veneer of “clinical necessity.”
The all‑day dosing model not only boosts sales but also creates dependency, ensuring patients stay locked into a costly cycle while newer, safer alternatives are quietly sidelined.
If you look closely at the FDA approval notes, you’ll see that several pivotal trials were funded by the same conglomerate that manufactures the drug, raising legitimate concerns about bias in the presented efficacy data.
Understanding this hidden agenda can empower patients to demand more transparent, evidence‑based prescribing practices.
Ramesh Kumar
October 28, 2025 AT 10:50While it’s true that industry influence can shape drug availability, the data still show that Procardia’s rapid onset can be clinically useful in specific scenarios, such as pre‑operative BP control.
Balancing efficacy with side‑effect profiles remains key, and a shared decision‑making approach helps ensure patients receive the most appropriate therapy for their individual needs.