Warfarin: What It Is, How It Works, and What You Need to Know
When you take warfarin, a prescription blood thinner used to prevent dangerous clots in the heart, legs, or lungs. Also known as Coumadin, it works by slowing down your body’s ability to form clots—critical if you have atrial fibrillation, a replaced heart valve, or a history of deep vein thrombosis. But warfarin isn’t like other pills. It doesn’t just work and you’re done. It needs constant checking, and small changes in your life can throw it off balance.
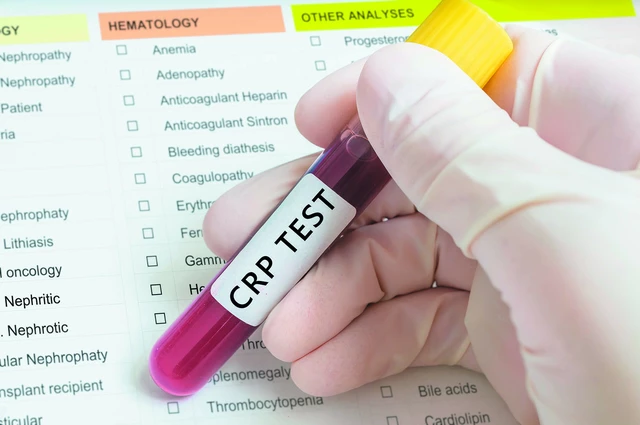
That’s where INR monitoring, a blood test that measures how long it takes your blood to clot comes in. Your doctor sets a target range—usually between 2.0 and 3.0—for your INR. If it’s too low, clots can form. Too high, and you risk serious bleeding. That’s why people on warfarin get blood tests every few weeks, or even use home monitors. Your diet matters too. Foods high in vitamin K—like spinach, kale, and broccoli—can make warfarin less effective. You don’t have to avoid them, but you need to keep your intake steady. And don’t forget other meds. Antibiotics, painkillers, even some herbal supplements can change how warfarin works. That’s why keeping a full list of everything you take, including over-the-counter stuff, is non-negotiable.
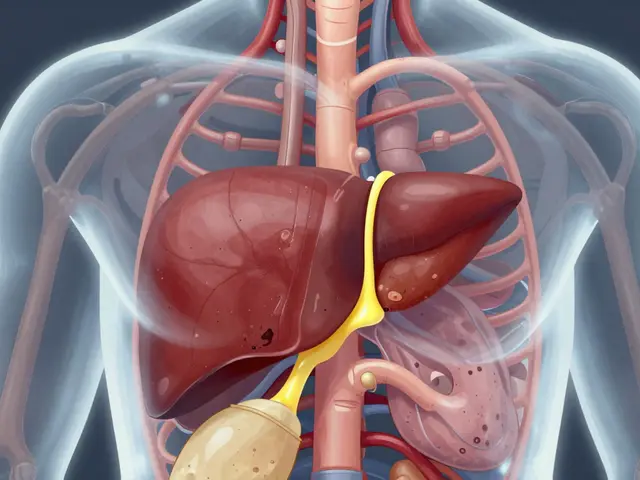
Anticoagulation therapy, the medical term for treatment with blood thinners like warfarin isn’t just about popping a pill. It’s about awareness. You need to know the signs of bleeding—unusual bruising, nosebleeds that won’t stop, red or dark urine, or headaches that feel different. A fall or bump that used to mean a bruise might now mean internal bleeding. And if you’re scheduled for surgery or a dental procedure, you must tell your provider you’re on warfarin. They might adjust your dose or pause it temporarily. This isn’t scare tactics—it’s how people stay safe.
Warfarin has been around for decades, but it’s still one of the most common blood thinners used worldwide. Newer options like apixaban or rivaroxaban don’t need regular blood tests, but they’re not right for everyone. If you’re on warfarin, it’s likely because your situation needs that level of control. The good news? With the right monitoring, diet habits, and communication with your care team, you can live well on it. You don’t have to live in fear. You just have to be informed.
Below, you’ll find real-life guides on how to track your INR, what to do when levels are off, how other meds interact with warfarin, and how to spot trouble before it becomes an emergency. These aren’t theory pieces—they’re tools people use every day to stay safe and in control.

Blood Thinner Overdose and Internal Bleeding: What to Do Immediately
Know the signs of blood thinner overdose and internal bleeding. Learn what to do immediately, how hospitals treat it, and how to prevent it from happening again.