Sodium Imbalance: Causes, Symptoms, and What You Need to Know
When your body’s sodium imbalance, a condition where blood sodium levels fall outside the normal range, either too low (hyponatremia) or too high (hypernatremia). It’s not just about salt on your food—it’s about how your kidneys, hormones, and fluids work together to keep things balanced. Sodium is one of the main electrolytes your body needs to control fluid levels, nerve signals, and muscle function. Even small shifts can make you feel off—headaches, nausea, confusion, or even seizures in severe cases.
Many things can throw off your sodium levels. diuretics, medications that make you pee more to reduce fluid buildup are a common culprit, especially loop diuretics like furosemide. They flush out sodium along with water, which can lead to hyponatremia, dangerously low sodium in the blood, often from too much water intake or excessive fluid loss. On the flip side, hypernatremia, high sodium levels usually caused by not drinking enough water or losing fluids through sweat, vomiting, or diarrhea, hits older adults and people with limited access to fluids harder. Kidney disease, heart failure, and even some hormone disorders like SIADH can also mess with sodium regulation.
What’s interesting is how often sodium imbalance shows up alongside other conditions you might not connect. For example, people on long-term diuretics for high blood pressure or swelling often need regular blood tests to catch sodium drops before symptoms get bad. And if you’re taking meds like fludrocortisone, a steroid used for adrenal insufficiency that helps the body hold onto sodium, your levels can swing if the dose isn’t right. Even something as simple as drinking too much water after a long run—or not drinking enough when you’re sick—can tip the scale.
You won’t always feel it coming. Some people with mild sodium imbalance feel nothing at all. Others get dizzy, weak, or confused without realizing it’s their sodium. That’s why tracking symptoms and knowing your meds matters. If you’re on diuretics, have kidney issues, or take steroids like fludrocortisone, your doctor should check your sodium levels regularly. And if you’re drinking a lot of water but still feeling tired, it’s worth asking if your sodium could be low.
Below, you’ll find real-world guides on how medications like diuretics affect electrolytes, how steroid treatments impact sodium balance, and what to watch for when managing chronic conditions that put you at risk. These aren’t just theory—they’re lessons from people who’ve been there.

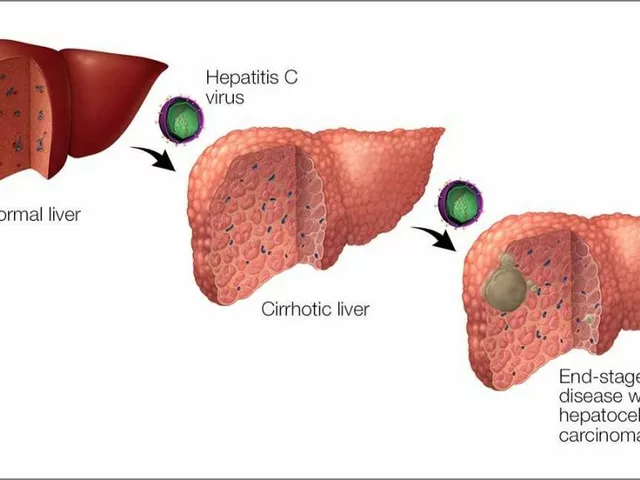
How Hyponatremia Impacts Heart Failure and What to Do About It
Learn how low blood sodium ties into heart failure, its symptoms, diagnosis, and treatment steps to manage fluid overload and improve outcomes.