Relapsing‑Remitting Disease: What You Need to Know
If you’ve heard the term “relapsing‑remitting disease” and feel confused, you’re not alone. It usually refers to a pattern where symptoms flare up (relapse) and then improve for a while (remission). The most common example is relapsing‑remitting multiple sclerosis (RRMS), but other conditions can show the same rhythm.
Understanding this back‑and‑forth helps you spot warning signs early, plan treatments, and keep daily life as normal as possible. Below we break down the basics, what to watch for when a relapse hits, and how modern therapies can smooth out those ups and downs.
Key Symptoms & How They Flare
A relapse often feels like old symptoms returning stronger or new problems showing up suddenly. Common signs include:
- Numbness or tingling in arms, legs, or face
- Blurred vision or eye pain
- Muscle weakness that makes walking hard
- Fatigue that won’t go away with rest
- Balance problems and frequent falls
These episodes can last days to weeks. What’s useful is tracking them in a simple notebook or phone app: note the date, what triggered it (like stress or infection), and how long it lasted. Over time you’ll see patterns that your doctor can use to adjust medication.
Don’t wait for a full relapse before seeking help. Early treatment with steroids or other fast‑acting drugs often shortens the attack and limits nerve damage. If you notice new symptoms, call your neurologist right away – quick action makes a big difference.
Treatment Paths and Everyday Management
There are two main goals: stop relapses from happening and keep disability low. Disease‑modifying therapies (DMTs) such as interferon injections, oral pills like fingolimod, or newer infusion drugs work by calming the immune system.
Choosing a DMT depends on your lifestyle, how active the disease is, and any other health issues you have. Some people prefer a weekly injection; others go for an IV infusion every few months because it fits their schedule better. Talk with your doctor about side‑effects, monitoring requirements, and insurance coverage.
Beyond meds, everyday habits matter a lot:
- Stay active. Light exercise – walking, swimming, yoga – improves strength and mood without overdoing it.
- Watch vitamin D levels. Low vitamin D is linked to more relapses. A daily supplement can be a simple guard.
- Manage stress. Stress spikes immune activity, which may trigger a flare. Mindfulness apps or short breathing breaks help keep calm.
- Get enough sleep. Quality rest supports nerve repair and reduces fatigue.
If you travel, plan ahead: carry your medication list, know where the nearest pharmacy is, and have a backup supply in case of delays. Many online pharmacies listed on our site offer discreet delivery to keep your treatment uninterrupted.
Finally, stay connected with a support community. Sharing experiences with others who live with relapsing‑remitting disease can give you practical tips that doctors don’t always mention – like the best ways to handle injection sites or how to talk to employers about flexible work hours.
Living with a relapsing‑remitting condition means expecting the unexpected, but with solid knowledge and a proactive plan, you can keep those surprise attacks to a minimum. Browse the articles on this page for deeper dives into specific drugs, coping strategies, and real‑world stories from people who’ve turned their relapses into manageable chapters of life.
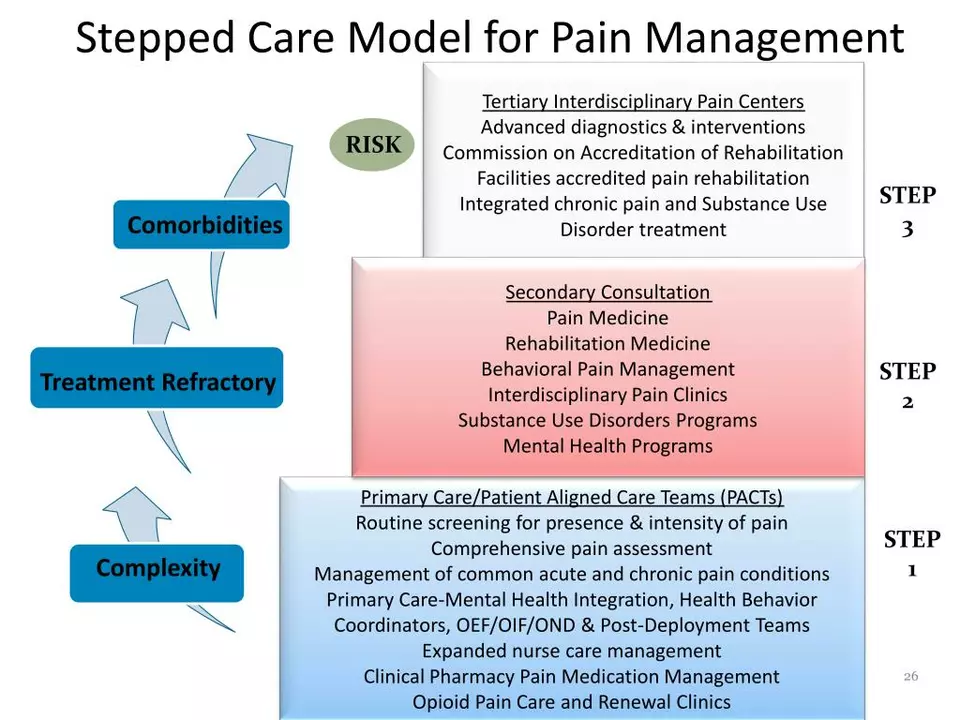
Managing Pain in Relapsing-Remitting Disease: Tips and Techniques
Managing pain in relapsing-remitting diseases can be challenging, but I've found several tips and techniques that have helped me cope. Firstly, staying in tune with my body and maintaining open communication with my healthcare team has been crucial. Secondly, incorporating relaxation techniques like deep breathing and meditation has been a game-changer in managing stress and pain. Additionally, maintaining a balanced diet and engaging in regular physical activity has significantly improved my overall well-being. Lastly, seeking support from friends, family, or support groups has been essential in managing my emotions and staying positive during difficult times.