Medication Safety: Protect Yourself from Errors, Interactions, and Side Effects
When you take a medication, you’re trusting that it’s safe, effective, and properly labeled—but medication safety, the practice of preventing harm from drugs through proper use, monitoring, and communication. Also known as drug safety, it’s not just about following instructions—it’s about knowing what to watch for, when to speak up, and how to spot hidden dangers. Too many people assume their doctor or pharmacist has it all figured out. But the truth? Over 7 million medication errors happen in the U.S. every year, and most never get reported because patients don’t know how or think it won’t matter.
That’s why black box warnings, the FDA’s strongest alert for life-threatening risks on prescription drugs. Also known as boxed warnings, they appear on drugs like blood thinners, antidepressants, and certain diabetes meds matter. These aren’t scare tactics—they’re red flags you need to understand. If your pill has one, you need to know the signs of trouble: unexplained bruising, sudden dizziness, confusion, or bleeding that won’t stop. And if you’re on blood thinner overdose, a dangerous condition where anticoagulants like warfarin or DOACs cause internal bleeding. Also known as anticoagulant emergency, it requires immediate action, you can’t wait for symptoms to get worse. Your INR levels, your peak flow numbers, your time in range—these aren’t just lab results. They’re your early warning system.
Medication safety also means knowing how your drugs talk to each other. Fish oil and aspirin? Most people think they’re harmless together—but they both thin the blood. Ranitidine was pulled because of cancer risks. Diuretics can wreck your electrolytes. Generic drug shortages? They’re not random. They come from factories in just two countries, with no backup plan. And if you’re seeing five different doctors? You’re one missed note away from a dangerous mix. That’s why keeping a real, updated list of everything you take—down to the dose and time—isn’t optional. It’s your lifeline.
You don’t need to be a medical expert to stay safe. You just need to know what questions to ask, what symptoms to track, and when to push back. The posts below give you exactly that: step-by-step guides on reporting errors, understanding warnings, managing blood thinners, avoiding interactions, and speaking up when something feels off. No jargon. No fluff. Just what works.
How to Store Prescription Labels and Leaflets for Future Reference
Keep prescription labels and leaflets organized to avoid dangerous medication errors. Learn how to store them safely in binders or apps, what to save, and why this simple habit could save your life.
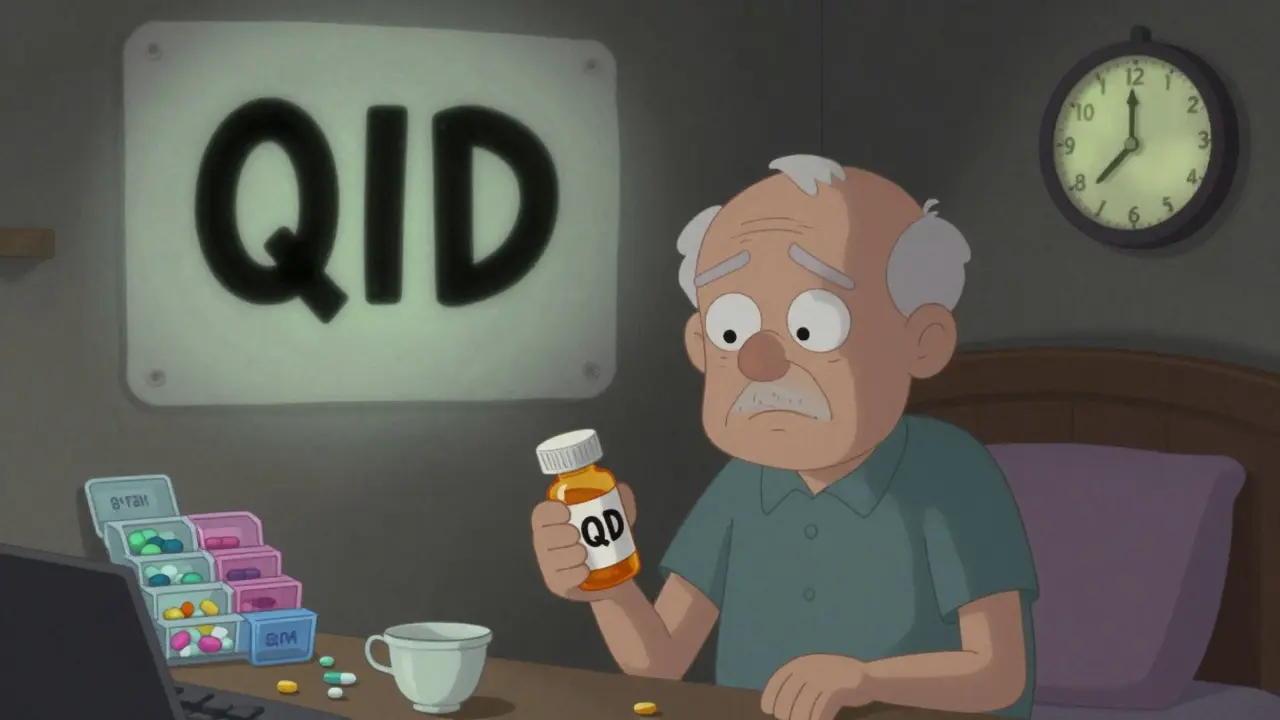
QD vs. QID: How Prescription Abbreviations Cause Dangerous Medication Errors and How to Stop Them
QD and QID are dangerous medical abbreviations that cause deadly dosing errors. Learn why they're still used, how they confuse patients and providers, and the simple, proven way to prevent mistakes.

Medication Safety at Night: How to Avoid Errors When You're Tired
Night shifts increase medication errors by 12.1%. Fatigue impairs memory, attention, and communication-making mistakes more likely. Learn how sleep deprivation, sedating meds, and poor scheduling put patients at risk-and what actually works to stop it.

Barcode Scanning in Pharmacies: How It Prevents Dispensing Errors
Barcode scanning in pharmacies prevents deadly medication errors by verifying the right patient, drug, dose, route, and time. Used in 78% of U.S. hospitals, it cuts errors by up to 93%-but only if used correctly.





