When you're on blood thinners - whether it's warfarin, apixaban, rivaroxaban, or dabigatran - the goal is simple: stop dangerous clots from forming. But there’s a dark side to that benefit. Severe bleeding is the most feared complication, and it doesn’t always come with warning signs. In fact, many people don’t realize they’re bleeding until it’s too late. Around 3.1% of people starting a direct oral anticoagulant (DOAC) for atrial fibrillation will have a major bleed within the first year. Half of those happen even when they’re on a low dose. And the scariest part? Sixty-one percent of these events occur within the first three months.
Why Blood Thinners Can Cause Life-Threatening Bleeding
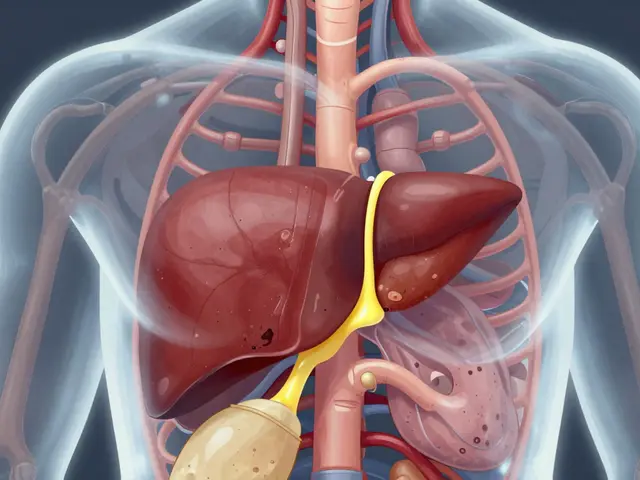
Blood thinners don’t actually make your blood thinner. They slow down the clotting process. Warfarin blocks vitamin K, while DOACs like apixaban and rivaroxaban block specific clotting factors. That’s good for preventing strokes. But if you cut yourself, fall, or develop an ulcer, your body can’t seal the damage quickly. The result? Uncontrolled bleeding. The risk isn’t random. Certain factors make it much worse. Age over 80? Your risk of major bleeding jumps to more than four times higher than someone under 60. Kidney problems? That triples your risk. Taking aspirin or clopidogrel along with your blood thinner? You’re doubling your chance of bleeding. And if you’ve bled before - even a small nosebleed that lasted too long - your risk of another major bleed is over four times higher. Not all blood thinners are the same. Apixaban has the lowest bleeding rate among DOACs - just 2.13% per year compared to 3.09% for warfarin. Rivaroxaban carries a higher risk of stomach bleeding, especially in people who’ve had ulcers before. Dabigatran can cause more bleeding in the gut. And warfarin? It’s unpredictable. Your INR level has to be checked every week at first, and even then, it can swing out of range. A single high INR above 5 can send you to the ER.The 12 Red Flags That Mean Immediate Medical Help Is Needed
Most people don’t know what severe bleeding looks like until it’s too late. It’s not always a gushing wound. Often, it’s quiet. Internal. Slow. Here’s what to watch for:- Nosebleeds lasting longer than 10 minutes, even if you’re pinching your nose
- Urine that turns red, pink, or brown - like cola
- Black, tarry, or sticky stools - a sign of bleeding in your stomach or intestines
- Unexplained bruising, especially large patches on your arms or legs
- Coughing up blood or vomiting blood (even if it’s just a little)
- A sudden, severe headache - like the worst one you’ve ever had
- Dizziness, weakness, or feeling like you’re going to pass out
- Blurred vision or double vision
- Unusually heavy or prolonged menstrual bleeding
- Swelling, pain, or tightness in a joint after a minor bump
- A cut that won’t stop bleeding after 15 minutes of pressure
- Feeling cold, clammy, or confused - signs your body is going into shock
One patient on Reddit described noticing black stools for three days before collapsing. By the time he got to the ER, he’d lost enough blood to need two units. He didn’t think it was serious. He wasn’t alone. A Mayo Clinic survey found 42% of patients had a bleeding event in their first year - and 28% didn’t realize it was serious until they were already in trouble.
What Happens When You Go to the ER With a Bleeding Emergency
If you show up with any of these signs, time is everything. The first thing they’ll do is check your blood pressure and heart rate. If you’re dizzy or pale, they’ll assume you’re losing blood. They’ll start an IV, give you fluids, and order a full blood count. If your hemoglobin has dropped more than 5 g/dL - or you need more than four units of blood - it’s classified as a major bleed. For warfarin users, they’ll give vitamin K and fresh frozen plasma to reverse the effect. For DOACs, it’s more complicated. If you’re on dabigatran, they’ll use idarucizumab - a $3,500 antidote that works in minutes. If you’re on rivaroxaban or apixaban, they’ll use andexanet alfa - a $12,500 treatment that’s not always available outside big hospitals. In the UK, not every A&E department keeps these drugs on hand. That’s why delays matter. Intracranial bleeding - bleeding in the brain - is the deadliest. It kills up to 15% of people who have it. That’s why a sudden headache or vision change isn’t something to wait on. Even if you think it’s just a migraine, get checked. A CT scan takes five minutes. Waiting an hour could cost you your life.
Why the First 90 Days Are the Most Dangerous
The first three months on any blood thinner are the most risky. Why? Your body is adjusting. Your kidneys are learning how to clear the drug. Your liver is processing it differently. And if your dose is too high - even slightly - you’re in danger. A 2024 study found that patients with the highest drug levels in their blood during the first month had more than three times the risk of bleeding. That’s why new guidelines now recommend checking DOAC levels 2-4 weeks after starting. The FDA approved the first point-of-care test for this in January 2024. It’s not yet standard everywhere, but clinics in Birmingham and London are starting to use it for older patients, those with kidney issues, or anyone who’s had a prior bleed. Doctors now know: if you’re over 75, have kidney trouble, or have had a bleed before, you need more than just a prescription. You need a plan. That’s why the NHS now uses the HAS-BLED score. If your score is 3 or higher, you get extra education, more frequent check-ins, and sometimes a lower dose.How to Protect Yourself - Practical Steps Everyone Should Take
You can’t avoid all risk. But you can drastically reduce it.- Know your meds. Know the name, dose, and why you’re taking it. Keep a list in your wallet or phone.
- Get your bleeding risk score. Ask your doctor for your HAS-BLED score. If it’s 3 or above, insist on a safety plan.
- Ask about DOAC levels. Especially if you’re over 70 or have kidney disease. A simple blood test 3-4 weeks in can save your life.
- Never skip follow-ups. If you’re on warfarin, get your INR checked every week for the first month. Don’t skip. Don’t delay.
- Carry a medical alert card. It should say what you’re on, your dose, and your doctor’s contact. Many pharmacies in the UK offer free ones.
- Teach someone. Make sure your partner, adult child, or close friend knows the 12 warning signs. You might not be able to call for help if you’re bleeding internally.
- Avoid NSAIDs. No ibuprofen, no naproxen. Use paracetamol instead - it’s safer with blood thinners.
- Wear non-slip shoes. Falls are a top cause of bleeding in older adults. A simple slip on a wet floor can lead to a brain bleed.
What’s Next? New Drugs, Better Safety
The future is starting to look brighter. Two new drugs - milvexian and asundexian - are in late-stage trials and show 20-25% less bleeding than current options, without losing their ability to prevent strokes. A universal reversal agent called Ciraparantag is also being tested. If it works, it could reverse all DOACs with one shot, costing around $8,500 per dose. But here’s the hard truth: no drug will ever be perfectly safe. The real solution isn’t just better medicine - it’s better awareness. Patients need to know that a nosebleed that won’t stop isn’t just annoying. A black stool isn’t just from food. A sudden headache isn’t just stress. The system is improving. But until you’re the one bleeding - you won’t know how fast things can go wrong.Can I still take aspirin if I’m on a blood thinner?
No - not unless your doctor specifically tells you to. Aspirin is an antiplatelet drug, and combining it with anticoagulants like warfarin or DOACs doubles your risk of major bleeding. Even low-dose aspirin (75mg) increases bleeding risk. If you’re on a blood thinner, use paracetamol for pain instead. Always check with your pharmacist or doctor before taking any new medication, including over-the-counter ones.
How long should I wait before calling an ambulance for a nosebleed?
If it lasts longer than 10 minutes despite pinching your nose and leaning forward, call 999. Don’t wait. Don’t try to wait it out. Bleeding from the nose can be a sign of something deeper - especially if you’re on anticoagulants. If you feel dizzy, weak, or your heart is racing while it’s happening, that’s a red flag. Emergency teams are trained to handle this. They can stop the bleed quickly and check for internal blood loss.
Do DOACs need regular blood tests like warfarin?
Normally, no. DOACs like apixaban and rivaroxaban don’t require routine blood tests because they work predictably. But if you’re over 75, have kidney problems, or have had a bleed before, your doctor may order a special test to measure your drug level. A new point-of-care test approved in early 2024 can check this in under 20 minutes at your clinic. It’s not standard yet, but it’s becoming more common for high-risk patients.
What should I do if I fall and hit my head while on blood thinners?
Go to the ER immediately - even if you feel fine. A head injury can cause bleeding inside the skull that doesn’t show symptoms right away. You might feel okay for hours, then suddenly get a headache, vomit, or become confused. That’s when it’s too late. A CT scan can catch internal bleeding early. Don’t wait. Don’t assume you’re fine. Your doctor will tell you to treat every head bump as a potential emergency.
Are there any foods I need to avoid with DOACs?
Unlike warfarin, DOACs aren’t affected by vitamin K-rich foods like spinach, broccoli, or kale. You don’t need to count your greens. But you should avoid grapefruit and Seville oranges - they can interfere with how your body processes some DOACs, especially rivaroxaban. Alcohol can also increase bleeding risk, so limit it to no more than one drink a day. Always ask your pharmacist about interactions with supplements - some herbal products like ginkgo, garlic, or ginger can thin your blood too.
Can I stop my blood thinner if I’m worried about bleeding?
Never stop without talking to your doctor. Stopping suddenly can cause a clot to form - which could lead to a stroke, heart attack, or pulmonary embolism. The risk of clotting is often higher than the risk of bleeding, especially if you have atrial fibrillation or a mechanical heart valve. If you’re scared, talk to your GP or anticoagulation clinic. They can adjust your dose, check your kidney function, or switch you to a safer option. But don’t quit cold turkey.






jonathan soba
January 28, 2026 AT 15:55Let’s be real - this post reads like a pharmaceutical ad with a side of fearmongering. The HAS-BLED score? Useful. But the way they frame every nosebleed as a death sentence? That’s not education, that’s anxiety salesmanship. I’ve been on apixaban for 3 years. Had two nosebleeds. Both stopped in 4 minutes. I didn’t go to the ER. I didn’t die. The system’s rigged to make you paranoid so you keep taking the pills.
And don’t get me started on the $12,500 reversal agents. If you’re in rural Wales or Nebraska, you’re just screwed. That’s not healthcare. That’s a lottery.
Also - why is no one talking about how DOACs are marketed as ‘safer’ while the real data shows they’re just different? Warfarin’s messy, but at least you can test it. DOACs? Black box. You’re flying blind.
And yes, I know I’m the guy who says ‘just don’t take them.’ But if your doctor didn’t sit down with you for 20 minutes and go over the risks? They’re not your doctor. They’re a script writer.
matthew martin
January 28, 2026 AT 19:49Man, this is one of those posts that makes you feel like you’re reading a medical thriller written by someone who’s seen too many ER episodes. But honestly? It’s 90% dead-on.
I’m a nurse in Arizona, and I’ve seen the ‘I thought it was just a headache’ crowd come in too late - more times than I can count. The black stools? The unexplained bruising? Those aren’t myths. They’re red flags painted in neon.
What this post doesn’t say enough is that the real hero here isn’t the drug - it’s the patient who knows their body. The guy who says ‘wait, my knee’s swollen after tripping over the rug?’ - that’s the guy who lives.
Also, shoutout to the NHS HAS-BLED score. Finally, someone’s treating risk like a math problem, not a guess.
And yes - grapefruit is the silent saboteur. I’ve seen it ruin INRs and DOAC levels. Just say no to citrus that looks like it’s auditioning for a citrus commercial.
Chris Urdilas
January 30, 2026 AT 12:51So let me get this straight - you’re telling me I can’t take ibuprofen for my back pain, I can’t drink my evening gin and tonic, I can’t even eat a grapefruit without risking a ‘major bleed’... but I’m supposed to be grateful because my blood is ‘thinner’ now?
Look, I get it. Strokes are scary. But this post reads like a PSA written by a hospital marketing team on Adderall.
Also - ‘carry a medical alert card’? Bro, I’ve got a wallet with a QR code that links to my entire medical history. And I still forgot to tell my Uber driver I’m on a blood thinner when I passed out in the backseat. (I didn’t. But I almost did.)
Point is: awareness is good. Fear is not. We’re not all gonna die from a nosebleed. But yeah - maybe don’t start parkour after your first dose.
Irebami Soyinka
January 30, 2026 AT 18:43Americans think they’re so smart with their ‘DOACs’ and ‘HAS-BLED scores’ - but in Nigeria, we don’t need fancy algorithms to know when blood is leaking. We know because the person turns pale, collapses, and we carry them to the hospital on a bicycle.
My uncle took warfarin for AFib. He didn’t know about INR. He didn’t have a card. He didn’t even have a fridge to keep his meds cold. He died in a taxi because no one knew what ‘black stool’ meant.
You think this post is scary? Try living where the nearest clinic is 30km away and the doctor charges $50 just to say ‘you’re bleeding.’
Stop romanticizing Western medicine. We don’t need more tests. We need more access. More doctors. Less $12,500 antidotes that only rich people can afford.
And yes - I’m angry. Because people die here every day because your ‘guidelines’ don’t reach them.
❤️ #NigeriaStillBleeding
doug b
February 1, 2026 AT 10:08This is gold. Real talk: if you’re on a blood thinner, you’re not just a patient - you’re a detective. Your body’s sending you clues. A bruise? A weird headache? A nosebleed that won’t quit? That’s your body screaming. Learn the language.
And listen - your doctor isn’t your enemy. But if they hand you a script and say ‘take this’ without asking about your falls, your diet, your kidney function - find a new one.
Carry the card. Tell someone. Skip the NSAIDs. Test your levels if you’re over 70. Simple. Not glamorous. But it saves lives.
I’ve seen too many people wait ‘just one more day.’ Don’t be that person. Your future self will thank you.
And yes - grapefruit is the devil. Avoid it like your ex’s texts.
Mindee Coulter
February 2, 2026 AT 08:51Rhiannon Bosse
February 2, 2026 AT 12:54Okay but… what if the whole blood thinner industry is just a giant money machine?
Think about it. We used to have warfarin - cheap, effective, monitored. Now? Five different DOACs, all $400/month, no routine testing, and you need a $12,500 antidote if you bleed? That’s not medicine. That’s a subscription service.
And don’t get me started on the ‘point-of-care test’ - approved in Jan 2024? Yeah, and it’s only in 3 hospitals in the UK. Meanwhile, your insurance won’t cover it unless you’re ‘high risk’ - which means you have to bleed first to qualify.
They’re not trying to save you. They’re trying to sell you a better version of the same poison.
And the ‘12 red flags’? That’s just fear marketing. You’re supposed to panic every time you sneeze.
Who profits? Pharma. Who pays? You. Who dies? The people who can’t afford the antidote.
Just saying - maybe don’t trust the system. Trust your gut. And maybe ask your doctor: ‘what would you do if this was your mom?’
James Dwyer
February 3, 2026 AT 19:45I’m 76 and on apixaban. I’ve been walking my dog every morning for 10 years. I haven’t fallen once. I take my meds. I know my signs. I carry my card. I told my daughter what to look for.
This post? It’s not scary. It’s empowering. Knowledge is armor.
I’m not afraid of bleeding. I’m afraid of not knowing. And now I know.
Thanks for this. Seriously. I printed it out and put it on my fridge.
Jeffrey Carroll
February 4, 2026 AT 23:41While the information presented is clinically accurate and well-structured, the tone risks inducing unnecessary anxiety in patients who may not be at elevated risk. The emphasis on catastrophic outcomes, while valid in extreme cases, may lead to non-adherence due to fear. A more balanced framing - emphasizing risk stratification and patient autonomy - would better serve the intended audience. The inclusion of practical, actionable steps is commendable and aligns with contemporary patient-centered care models. Further dissemination of point-of-care testing should be prioritized in resource-limited settings to ensure equitable access to safety monitoring.
Phil Davis
February 6, 2026 AT 02:56So… if I’m on rivaroxaban and I get a nosebleed, I’m supposed to call 999? What if I’m in the middle of a Zoom meeting? Do I just hang up and scream?
Look - I get it. Bleeding’s bad. But this post reads like a horror movie trailer. ‘You think your headache’s stress? Nope. It’s a brain bleed. Also, your grapefruit juice is plotting against you.’
Maybe tone it down a notch? I’m not saying don’t warn people - I’m saying don’t turn every minor symptom into a countdown to death.
Also - ‘don’t stop your meds’? Yeah, I know. But if your doctor won’t even check your kidney function before prescribing? That’s the real problem.
Mel MJPS
February 7, 2026 AT 12:11I just started apixaban last month and I’ve been so scared. This post actually helped me feel less alone. I told my husband the 12 signs last night and we laughed about the grapefruit thing - now he’s hiding my orange juice. 😅
Thanks for making it real. Not just scary. Real.
Katie Mccreary
February 8, 2026 AT 22:24SRI GUNTORO
February 9, 2026 AT 01:37People in the West always think they have the monopoly on wisdom. In India, we’ve been managing anticoagulation for decades with warfarin and home INR monitors. We don’t need $12,500 drugs. We need education. We need doctors who speak our language. We need to stop treating patients like lab rats.
And yes - you should avoid NSAIDs. But you should also avoid believing every American blog post is gospel.
Stop exporting fear. Start exporting solutions.