Every year, tens of thousands of people end up in emergency rooms because they took a supplement with their medicine-and didn’t realize it could be dangerous. It’s not just about vitamins. It’s about what’s in those bottles labeled ‘natural’ or ‘herbal’ that you’re popping alongside your blood pressure pill, antidepressant, or blood thinner. The truth? Supplement and medication interactions are real, often silent, and rarely discussed by doctors during a 10-minute visit.
Why This Isn’t Just a ‘Natural’ Thing
People assume if it’s sold in a health store, it’s safe. That’s the biggest mistake you can make. Supplements don’t go through the same testing as prescription drugs. The FDA doesn’t approve them before they hit shelves. That means a bottle of St. John’s wort might have 50% more of the active ingredient than the label says-or it might be mixed with something completely different. A 2022 Government Accountability Office report found that 70% of supplement labels misstate ingredient amounts. That’s not a typo. That’s a risk.And it’s not just about purity. It’s about how these substances react inside your body. Take St. John’s wort, for example. It’s marketed for mood support. But it triggers a chain reaction in your liver that can slash the effectiveness of your medication by up to 80%. That’s not a small drop. That’s enough to make your birth control fail, your transplant organ get rejected, or your HIV virus rebound. In one study, organ transplant patients on cyclosporine saw their drug levels drop by 50-60% after taking St. John’s wort. That’s not a theory. That’s documented in clinical trials.
What Happens When Supplements Meet Medicines
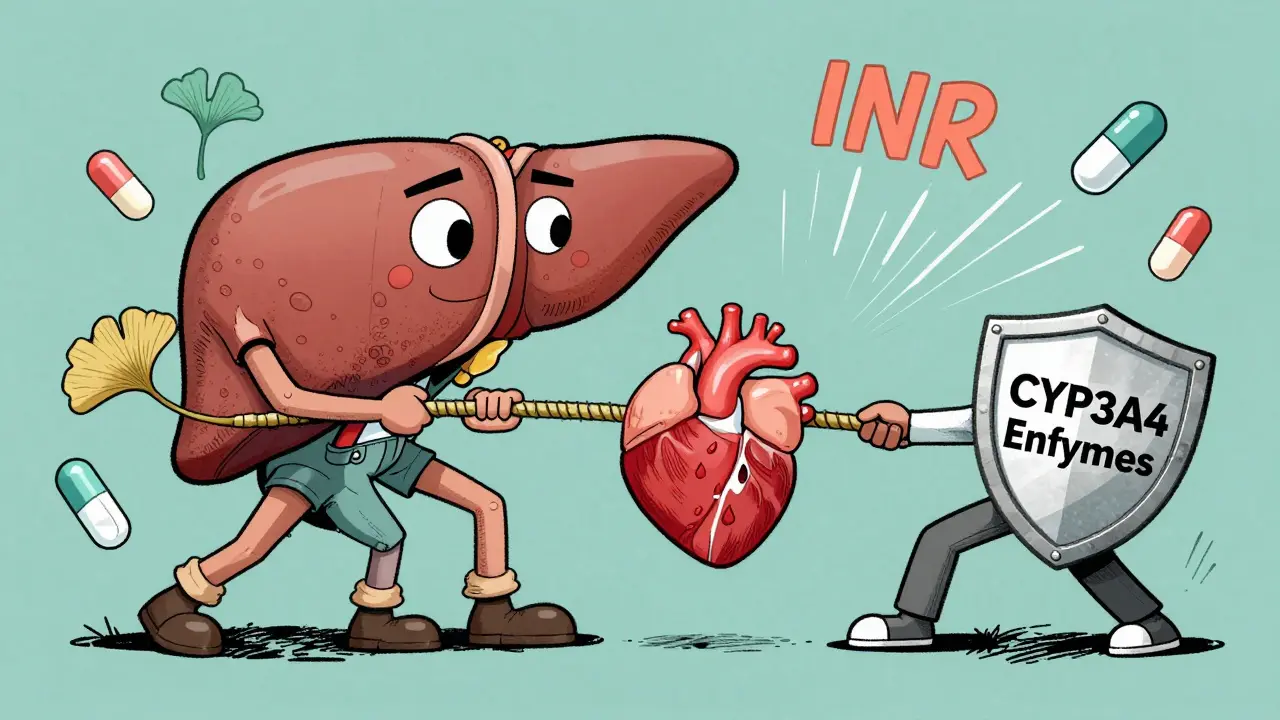
Your body breaks down drugs using enzymes-mostly a group called cytochrome P450. Some supplements mess with these enzymes. St. John’s wort turns them on full blast, flushing your meds out of your system too fast. Others, like grapefruit juice, shut them down, making your drugs build up to toxic levels. Then there’s the second kind of interaction: additive effects. Ginkgo biloba and warfarin? Both thin the blood. Together, they can push your INR into dangerous territory. One study found 15% of people on warfarin who added ginkgo saw their INR spike to 2.5-3.5. Normal is 2-3. Above 4? Risk of bleeding skyrockets.Vitamin E at doses over 400 IU daily can make warfarin work too well. Milk thistle? Often thought to be gentle, but it can interfere with liver-metabolized drugs like statins or some cancer meds. Even garlic supplements can increase bleeding risk during surgery. And don’t forget about hormonal birth control. St. John’s wort has been linked to 40-50% higher failure rates. Women have gotten pregnant because they didn’t know.
The High-Risk Supplements (And What to Avoid)
Not all supplements are created equal when it comes to danger. Experts classify them into tiers:- High-risk: St. John’s wort, goldenseal
- Moderate-risk: Ginkgo biloba, garlic, echinacea
- Lower-risk (with caution): Milk thistle, American ginseng, cranberry, valerian
St. John’s wort is the worst offender. It interacts with over 50 prescription drugs-including antidepressants, antivirals, heart meds, and immunosuppressants. The American Academy of Family Physicians says it’s the most dangerous OTC supplement because it interferes with more drugs than any other. If you’re on any of these, don’t touch it:
- Antidepressants (SSRIs like Prozac, Zoloft)
- HIV meds (like indinavir)
- Birth control pills
- Cyclosporine or tacrolimus (transplant drugs)
- Warfarin or other blood thinners
- Chemotherapy drugs
Even if you’ve taken it for years without issues, that doesn’t mean it’s safe. Your body changes. Your meds change. A new prescription could turn your old supplement into a hidden time bomb.
Seven Questions to Ask Before Taking Any Supplement
You don’t need to be a pharmacist to protect yourself. Just ask these seven questions before you swallow anything:- Does this supplement affect how my body processes my medication? Look for info on cytochrome P450 enzymes. If it says “induces” or “inhibits” liver enzymes, tread carefully. St. John’s wort induces CYP3A4-meaning it speeds up drug breakdown.
- Could this make my drug stronger or weaker? If your medication is for something life-critical-like blood pressure, seizures, or heart rhythm-even a small change can be dangerous. Ask: Has this been studied with my specific drug? Only 15% of supplements have real interaction data.
- Is there a risk of additive effects? Are you taking something that does the same thing as your medicine? Ginkgo + warfarin = more bleeding. Fish oil + blood thinners = same problem. Vitamin E + warfarin = higher bleeding risk.
- Has this been studied in people like me? Most studies are done on healthy young adults. If you’re over 65, have liver disease, or are on multiple drugs, the data might not apply. Ask your pharmacist.
- What should I monitor? If you’re on warfarin, you need regular INR checks. If you’re on HIV meds, viral load matters. If you’re on immunosuppressants, drug levels should be tracked. Know what numbers to watch.
- Is there a safer alternative? American ginseng has fewer interactions than Asian ginseng. Cranberry juice is safer than cranberry extract for people on blood thinners. Sometimes, skipping the supplement entirely is the best choice.
- What symptoms mean trouble? Watch for: confusion, rapid heartbeat, muscle stiffness, fever (signs of serotonin syndrome from mixing St. John’s wort with antidepressants). Unexplained bruising, nosebleeds, or dark stools? Could be bleeding from ginkgo or garlic with warfarin. Nausea, dizziness, or fainting? Could mean your blood pressure med got too strong.
Why Your Doctor Might Not Tell You
A 2022 study in JAMA Internal Medicine found doctors spend just 1.2 minutes talking about supplements during a typical 15-minute appointment. Most don’t ask. Many don’t know. Pharmacists are better trained-they screen for interactions during medication reviews-but only 32% of primary care doctors document supplement use in medical records. That means you’re the only one who can speak up.Don’t wait to be asked. Bring a list. Write down every pill, capsule, tea, or powder you take-even if you think it’s harmless. Say: “I’m taking this with my prescription. Can you check if it’s safe?”

What You Can Do Right Now
1. Stop guessing. If you’re on a critical medication-blood thinner, transplant drug, antidepressant, or HIV treatment-assume every supplement is risky until proven otherwise. 2. Check the FDA’s DSID-6 database. It’s a new, verified list of supplement ingredients. Not perfect, but better than nothing. 3. Use the LiverTox database. Run by the NIH, it shows which supplements have caused liver damage. Many people don’t realize herbal teas or detox blends can fry their liver. 4. Ask your pharmacist. They’re the experts on drug interactions. Walk in with your list. Most will check it for free. 5. Don’t trust marketing. “All-natural,” “pure,” “clinically proven”-these words mean nothing legally. Look for USP-verified labels. That means the product was tested for what’s inside.The Bottom Line
You wouldn’t mix bleach and ammonia and expect to clean your kitchen. But people do the same thing every day with supplements and medicines. The system isn’t designed to protect you. The burden falls on you. Don’t assume safety. Don’t assume your doctor knows. Don’t assume natural means harmless.St. John’s wort isn’t the only danger. Ginkgo, garlic, vitamin E, echinacea, even green tea extract-all can interfere. The key isn’t avoiding all supplements. It’s asking the right questions before you take one. Because when your medicine and your supplement collide, it’s not a debate. It’s a medical emergency waiting to happen.







Thomas Anderson
December 16, 2025 AT 12:13Just stopped taking my ginkgo after reading this. Had no idea it could mess with my blood thinner. Scary stuff.
Rulich Pretorius
December 17, 2025 AT 11:58This is one of those topics that gets buried under wellness fluff. People treat supplements like candy-‘it’s natural, so it’s harmless.’ But your liver doesn’t care if it’s from a tree or a lab. It just processes toxins. The fact that the FDA doesn’t regulate these before sale is a systemic failure. We’re all guinea pigs in a free-market experiment where profit trumps safety. And doctors? They’re overworked and undertrained on this. The burden shouldn’t be on patients to become pharmacologists just to stay alive.
It’s not about fear. It’s about responsibility. If you’re on anything critical-antidepressants, transplant meds, anticoagulants-you owe it to yourself to treat every supplement like a potential drug interaction until proven otherwise. That’s not paranoia. That’s basic self-preservation.
I’ve seen too many people assume ‘herbal’ means ‘safe.’ St. John’s wort isn’t some gentle mood booster. It’s a metabolic wrecking ball. It can turn your life-saving meds into useless water. And no, your cousin who’s been taking it for five years ‘with no problems’ isn’t evidence. Biology isn’t static. Your body changes. Your meds change. The supplement batch changes. One day, it all collapses.
Pharmacists are your real allies here. Walk in with a list. Don’t be shy. They’ve seen it all. And if your doctor doesn’t ask about supplements, ask them why not. That silence isn’t negligence-it’s negligence by design.
USP-verified labels? That’s your minimum bar. Anything else is gambling with your biology. And if you’re using ‘natural’ as a moral justification? That’s dangerous thinking. Poison ivy is natural too.
Dwayne hiers
December 17, 2025 AT 16:17St. John’s wort is a potent CYP3A4 and P-glycoprotein inducer, which significantly reduces plasma concentrations of substrates like cyclosporine, tacrolimus, and SSRIs via enhanced hepatic and intestinal metabolism. The clinical implications are non-trivial: subtherapeutic drug levels can lead to transplant rejection, treatment-resistant depression, or contraceptive failure. The GAO’s 70% mislabeling statistic underscores the lack of analytical validation in the supplement industry. Furthermore, ginkgo biloba’s flavonoid and terpene constituents inhibit platelet-activating factor, synergizing with anticoagulants to elevate INR beyond therapeutic range. Vitamin E at >400 IU/day exhibits anticoagulant properties via vitamin K antagonism, compounding warfarin’s effect. The LiverTox database, maintained by NIH, documents over 1,200 cases of herb-induced liver injury, with green tea extract and weight-loss blends being top contributors. Without mandatory pre-market bioequivalence testing, consumer risk remains unacceptably high.
Jonny Moran
December 19, 2025 AT 04:21I’m from a place where herbal remedies are part of daily life-no judgment. But this? This is the kind of info that could save someone’s life. I’ve seen grandmas take garlic pills ‘for heart health’ and end up in the ER after surgery. No one told them it thins blood. It’s not about shaming people for using natural stuff-it’s about giving them real tools. Talk to your pharmacist. Write down everything. Even that ‘harmless’ tea. Your body doesn’t care if it’s organic or not. It just reacts. And sometimes, it reacts hard.
Next time you’re at the pharmacy, ask the person behind the counter. They’re the unsung heroes here. They know what’s dangerous before you even walk in. Don’t wait for a crisis. Ask now. It’s not a dumb question. It’s the smartest thing you can do.
Sarthak Jain
December 19, 2025 AT 13:15bro i took st johns wort for like 2 yrs n never had an issue but now im on blood pressure med and i just read this… damn. i think im gonna stop. also ginkgo? i take that for memory. is it bad? like really bad? i dont wanna be dumb but i also dont wanna die.
Tim Bartik
December 20, 2025 AT 12:36Oh wow, so now we’re supposed to trust Big Pharma over grandma’s herbal tea? Typical American paranoia. Back in my day, people didn’t need a PhD to take a pill. You just trusted nature. Now everything’s a ‘risk.’ You think your ‘FDA-approved’ pills are clean? They’re full of chemicals no one’s even named yet. And don’t get me started on how they suppress real cures. This whole ‘check with your pharmacist’ thing? That’s just another way to make you pay for advice. Take your supplements. Live your life. Stop being scared of everything.
Sinéad Griffin
December 21, 2025 AT 19:44OMG I JUST REALIZED I’VE BEEN TAKING GINKGO WITH MY WARFARIN 😱 I’M SO GLAD I READ THIS BEFORE I HAD A STROKE 😭🙏 PLEASE SHARE THIS WITH EVERYONE!! 🚨
jeremy carroll
December 23, 2025 AT 17:17Man, I was gonna start taking turmeric for my knees. Now I’m not so sure. But hey, at least I’m reading up on it before I do something dumb. Thanks for the heads-up. You’re right-we gotta be our own advocates. I’m printing this out and taking it to my doc tomorrow.
Edward Stevens
December 25, 2025 AT 00:39So let me get this straight. The government lets snake oil be sold as medicine, doctors don’t ask about it, and now we’re supposed to be grateful for a blog post that tells us not to kill ourselves? Wow. What a system. I’m just here waiting for the day they make us sign a waiver before drinking water.
Daniel Thompson
December 26, 2025 AT 21:38As a medical professional, I must emphasize that supplement use is underreported in clinical settings due to patient omission, not clinician negligence. The data is clear: over 70% of patients do not disclose supplement use unless directly asked. This is not a failure of regulation-it is a failure of communication. Patients must be educated to proactively disclose all substances consumed, including teas, tinctures, and topical applications. The responsibility lies equally with the individual and the system.
Alexis Wright
December 27, 2025 AT 09:35Let’s be brutally honest: the supplement industry is a cult disguised as healthcare. It preys on the vulnerable, the desperate, the gullible. And the FDA? They’re asleep at the wheel because lobbyists pay for their silence. St. John’s wort isn’t just dangerous-it’s a symbol of everything wrong with American health culture. We’ve turned medicine into a spiritual experience. You don’t need a pill to ‘balance your energy.’ You need a doctor who knows biochemistry. And if your ‘natural remedy’ causes serotonin syndrome? That’s not a side effect. That’s a crime. Someone made money off your suffering. And they’re still selling it.
Don’t be fooled by ‘clinically proven’ labels. That’s just marketing jargon. No clinical trial for St. John’s wort was ever double-blind, placebo-controlled, and peer-reviewed to pharmaceutical standards. It’s a placebo with teeth. And you’re the one getting bitten.
Daniel Wevik
December 29, 2025 AT 04:57This is exactly the kind of clarity we need. Too many people think ‘natural’ equals ‘safe’-and that’s a dangerous myth. The body doesn’t care where a compound comes from. It cares about dosage, metabolism, and interactions. That’s why I always tell my clients: if you’re on anything critical, treat supplements like prescription drugs. Check the label. Look for USP. Ask your pharmacist. Don’t guess. Don’t assume. And if you’re unsure? Skip it. Your health isn’t worth the risk.
Knowledge is power. And right now, power is in your hands. Use it.
Rich Robertson
December 30, 2025 AT 02:00I’m from a country where herbal medicine is part of the culture. We’ve used ginseng, turmeric, and ashwagandha for centuries. But here’s the thing-we also knew our limits. We didn’t mix them with heart meds or antidepressants. We didn’t assume they were harmless. We had elders who knew what worked and what didn’t. Today, we’ve lost that wisdom. We buy supplements like snacks and hope for the best. This article? It’s not anti-traditional. It’s pro-responsibility. Respect your roots. But respect your biology more.
Natalie Koeber
January 1, 2026 AT 01:24Did you know the FDA is in bed with Big Pharma and the supplement industry? They’re all part of the same cartel. They want you scared of herbs so you’ll keep buying their patented drugs. St. John’s wort cures depression better than SSRIs-but they can’t patent a plant. That’s why they ban it in Europe. And ginkgo? It’s been used for thousands of years. The real danger is the chemicals in your ‘FDA-approved’ meds. They’re poisoning your liver slowly. This whole article? It’s a distraction. The real villain is the system. Not the herbs.
Rulich Pretorius
January 2, 2026 AT 06:08Interesting how the conspiracy crowd jumps in the second someone mentions regulation. The FDA doesn’t ban St. John’s wort because it’s not proven dangerous-it’s because it’s not proven *effective* enough to warrant approval. And yes, it’s legal because the DSHEA law of 1994 says supplements don’t need pre-market approval. That’s not a conspiracy. That’s a law passed by Congress. The problem isn’t that herbs are being suppressed-it’s that they’re being sold without proof they work or are safe. If you want herbal medicine to be respected, demand science. Not paranoia.