Most people think hearing aids go in your ear. But what if the solution doesn’t touch your ear at all? That’s the reality with bone-conduction hearing aids. These devices don’t amplify sound through the ear canal. Instead, they send vibrations straight through your skull bone to the inner ear, skipping the outer and middle ear completely. This makes them a game-changer for people who can’t use regular hearing aids because of chronic infections, birth defects, or blocked ear canals.
How Bone-Conduction Hearing Aids Actually Work
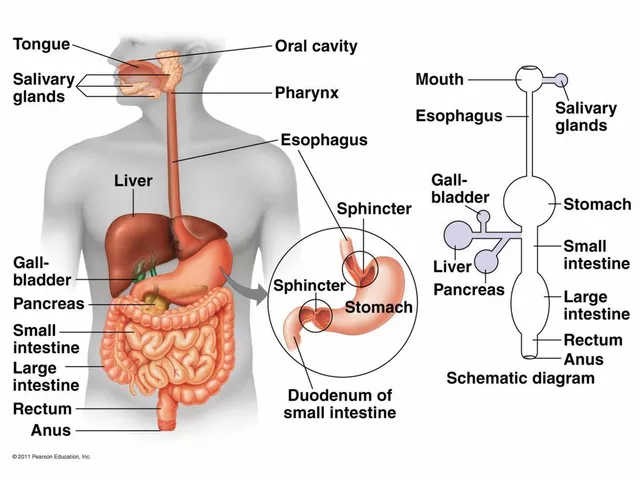
Sound normally travels through the air, hits your eardrum, and bounces through tiny bones in the middle ear before reaching the cochlea. But if any part of that path is blocked or damaged - like a malformed ear canal or scar tissue from repeated infections - sound can’t get through. That’s where bone conduction comes in.
These devices use a simple principle: bone conducts sound better than air. When a sound processor vibrates against your skull, those vibrations travel through the bone directly to the cochlea. It’s the same reason you hear your own voice differently when you speak - you’re hearing it through bone, not air.
The technology isn’t new. It started with Swedish surgeon Per-Ingvar Brånemark’s discovery in the 1950s that titanium fuses with bone. That led to the first Bone-Anchored Hearing Aid (BAHA) in 1977. Today, you’ve got two main types: percutaneous (with a metal post sticking through the skin) and transcutaneous (magnetic, no skin penetration).
Who Benefits Most From Bone-Conduction Devices
Not everyone needs one. These are designed for specific hearing loss types:
- Conductive hearing loss: When the outer or middle ear can’t pass sound. Common in people with chronic ear infections, earwax buildup that won’t clear, or congenital aural atresia (a birth defect where the ear canal didn’t form).
- Mixed hearing loss: A combo of conductive and sensorineural (nerve-related) loss. Bone conduction helps bypass the damaged part.
- Single-sided deafness (SSD): When one ear is completely deaf but the other works fine. Bone conduction sends sound from the deaf side to the good ear, helping you hear from all directions.
Studies show these devices improve speech understanding in noise by 20-35% for SSD patients. For people with congenital aural atresia, success rates hit 85-90%. If you’ve been told you can’t wear regular hearing aids because your ear canal is too narrow, infected, or malformed - this might be your only real option.
Percutaneous vs. Transcutaneous: The Key Differences
There are two main types of bone-conduction systems, and the choice comes down to trade-offs.
Percutaneous systems (like Cochlear’s BAHA Connect or Oticon’s Ponto 5) use a titanium implant fused to your skull bone. After 3-6 months of healing, a metal abutment sticks out through the skin. The sound processor clips right onto it. These give you the strongest signal - up to 50 dB of gain - and are best for severe hearing loss.
But there’s a catch: skin problems. About 28% of users get irritation, infection, or overgrowth around the abutment. Daily cleaning with 70% isopropyl alcohol is mandatory. A small percentage (8%) end up needing revision surgery.
Transcutaneous systems (like MED-EL’s Bonebridge or Cochlear’s BAHA Attract) use magnets. The implant sits under the skin, and the external processor holds on magnetically. No open wound. No daily cleaning. No visible post. The downside? Signal loss. Skin and tissue block some vibration, so max output is around 45 dB. That’s fine for mild to moderate loss, but not enough for severe cases.
Today, 63% of new implants are transcutaneous. Why? Because patients want invisible, low-maintenance solutions. Satisfaction with invisible systems is 92%, compared to 76% for visible abutments.

Cost, Surgery, and Recovery
These aren’t over-the-counter devices. You need surgery.
The procedure is minor - 30 to 60 minutes, under local anesthesia. Most people go home the same day. Recovery is quick: back to normal activities in 48 hours. But timing depends on the type.
- Percutaneous: Wait 3-4 months for the implant to fuse with bone before turning it on.
- Transcutaneous: Can be activated right after surgery.
Cost is steep. Implantable systems run $4,000-$7,000 per ear. That’s 2-3 times more than a top-tier air-conduction hearing aid. Insurance sometimes covers it - especially if you have documented medical reasons (like chronic infections or congenital deformities). The American Academy of Otolaryngology calls these devices "medically necessary" for qualifying cases.
Once you’re fitted, you’ll need 2-4 weeks to adjust. The sound feels different - more direct, sometimes metallic at first. Audiologists recommend simple listening exercises: start with quiet rooms, then move to noisy places. Many users say they hear birds, footsteps, or even their own breathing on the deaf side for the first time in years.
Real User Experiences
On Reddit’s r/Hearing, users with single-sided deafness report emotional breakthroughs. One wrote: "I heard a bird chirp from my deaf side for the first time in 15 years." Another said, "I finally stopped turning my head like a owl to catch conversations."
Positive feedback is common: natural sound quality, no ear canal pressure, no feedback whistles. People with chronic ear infections say they finally feel free from constant drainage and discomfort.
But complaints exist too. About 23% of users struggle with MRI compatibility. Most implants are made of titanium, which is safe, but the external processor or magnet can interfere with 1.5T or higher scanners. Some need surgery to remove the implant before an MRI - a painful, expensive hassle.
Another issue: processor detachment. Active users - runners, swimmers, people who wear helmets - report the magnet or clip coming loose. Newer models have stronger retention, but it’s still a concern.

What’s New in 2026
The field is evolving fast. In 2023, Cochlear launched the BAHA 6 Max with Bluetooth 5.3, 30-hour battery life, and direct streaming from phones. Oticon’s Ponto 5 SuperPower offers 50 dB gain and water resistance. MED-EL’s Bonebridge 3, launching in Q2 2024, uses AI to reduce background noise automatically.
The biggest trend? Moving away from visible abutments. Transcutaneous systems now make up 63% of new implants - up from 41% in 2019. Why? Fewer infections, better cosmetics, less maintenance.
The next leap? Fully implantable bone conduction devices - no external processor at all. Sonova’s prototype is in Phase III trials, with FDA submission expected by late 2024. Imagine a device that works like a pacemaker: everything hidden under the skin, controlled by an app. That’s the future.
When Bone Conduction Won’t Help
It’s not a magic fix. If your cochlea is severely damaged - say, sensorineural hearing loss worse than 55 dB - bone conduction won’t help. The device can send vibrations, but if the inner ear can’t process them, you won’t hear anything.
It also won’t fix tinnitus or balance issues. And if you’re not willing to commit to follow-up care - cleaning, adjustments, occasional repairs - you might regret it.
For most people with conductive or mixed loss, or SSD, it’s the best option they’ve had. But you need a full hearing test, a CT scan, and a consultation with an ENT specialist who’s experienced with these devices. Not every audiologist knows how to fit them properly.
Final Thoughts
Bone-conduction hearing aids aren’t for everyone. But for the right person - someone with blocked ears, a malformed canal, or single-sided deafness - they’re life-changing. They don’t just restore hearing. They restore normalcy: hearing your child’s voice from behind you, catching a car horn on your deaf side, not having to turn your head to understand someone.
The tech is mature, the results are proven, and the options are better than ever. If you’ve been told you can’t use a regular hearing aid, don’t accept that as the end of the line. Ask about bone conduction. It might be the solution you didn’t know existed.
Are bone-conduction hearing aids visible?
It depends on the type. Percutaneous systems have a small metal post sticking out of the skin behind the ear - it’s visible but discreet. Transcutaneous systems use magnets under the skin, so the external processor clips on and looks like a small behind-the-ear device. Many users say it’s nearly invisible, especially with newer models that come in skin-tone colors.
Can I wear these if I have chronic ear infections?
Yes - that’s one of the main reasons people choose them. Regular hearing aids sit in the ear canal and can trap moisture, worsening infections. Bone-conduction devices bypass the ear canal entirely, so they don’t irritate infected skin. Studies show 92% of people with chronic ear infections who couldn’t use traditional aids find bone conduction safe and effective.
Do these work for severe hearing loss?
It depends. Percutaneous systems (like BAHA Connect 6 or Ponto 5 SuperPower) can deliver up to 50 dB of gain, which helps with moderate to severe conductive or mixed loss. But if your inner ear (cochlea) is severely damaged - say, over 55 dB sensorineural loss - bone conduction won’t help. The vibrations can’t be processed. For severe sensorineural loss, cochlear implants are the better option.
Can I swim or shower with a bone-conduction hearing aid?
You can shower with most models - they’re water-resistant. But you must remove the external processor before swimming. Water pressure and chlorine can damage the electronics. Some newer transcutaneous systems, like the Ponto 5, are rated for swimming with a special waterproof cover. Always check your device’s IP rating and follow the manufacturer’s guidelines.
Will an MRI ruin my implant?
The titanium implant itself is MRI-safe. But the external processor and the magnet in transcutaneous systems can be pulled or heated by strong magnetic fields. Most hospitals require you to remove the external part before an MRI. For transcutaneous systems, some patients need minor surgery to remove the internal magnet before a 1.5T or higher scan - and then have it replaced afterward. Always tell your radiologist you have a bone-conduction implant before any scan.
How long do the batteries last?
Battery life varies by model. Most devices last 5-7 days on a single charge with moderate use. Newer models like the BAHA 6 Max offer up to 30 hours of continuous use. Rechargeable batteries are standard now - no more swapping tiny zinc-air batteries. Some systems even have fast charging: 10 minutes gives you 3 hours of use.
Can children use bone-conduction hearing aids?
Yes - and they’re often the best option for kids with congenital aural atresia or chronic ear infections. For very young children, a softband version is available. It’s a headband with the processor attached, worn like a headband. No surgery needed. Once they’re old enough (usually 5+), they can get an implant. Many children who use these devices catch up to their peers in speech and language development.
How do I know if I’m a candidate?
Start with a full hearing test from an audiologist who specializes in hearing loss types. If you have conductive or mixed loss, or single-sided deafness, you may qualify. Your ENT will likely order a CT scan to check your skull bone thickness and ear anatomy. If your ear canal is blocked, infected, or malformed - and traditional aids don’t work - you’re a strong candidate. Don’t assume you’re out of options. Ask for a bone-conduction evaluation.





Ian Long
January 9, 2026 AT 19:40Been using a Ponto 5 for two years now. The first time I heard my kid laugh from behind me? I cried in the grocery store. No joke. This thing didn’t just fix my hearing-it fixed my life.
Pooja Kumari
January 10, 2026 AT 01:53Okay but let’s be real-this tech is wild. I’m from India and my cousin had congenital aural atresia, no ear canal at all. She tried every hearing aid under the sun, got infections every other week. Then she got the Bonebridge. Now she listens to Bollywood music with her headphones ON and doesn’t even need volume. It’s like magic. I still don’t get how vibrations through bone work but I’m not questioning it anymore. Also, she’s dating now. No joke. Confidence level: maxed out.
Jacob Paterson
January 10, 2026 AT 15:38Of course it works. But why are we glorifying a $7k surgery when a $200 bone-conduction headset you clip on your glasses exists? You’re all acting like this is the second coming when it’s just a fancy workaround for lazy ENTs who don’t want to fix the root problem. Also, MRI hassle? Yeah, that’s on you for not researching before shelling out grandpa money.
Angela Stanton
January 11, 2026 AT 04:36Let’s unpack the ROI here. Percutaneous: 50 dB gain, 28% infection rate, 8% revision surgery. Transcutaneous: 45 dB gain, 0% skin breach, 92% satisfaction. The data’s clear-transcutaneous dominates on QoL metrics. But here’s the kicker: 63% adoption rate doesn’t mean it’s optimal, it means patients are prioritizing aesthetics over acoustics. We’re optimizing for invisibility, not auditory fidelity. That’s a societal problem disguised as a medical one.
Lindsey Wellmann
January 11, 2026 AT 19:45OMG I just got my BAHA 6 Max and I can hear my cat purring from the other room?? 😭💖 I’ve been deaf in one ear since I was 8 and I just heard a leaf fall on my balcony… I’m not okay. I’m not okay. I need to sit down. Someone send me tea. And maybe a therapist. 🫖😭
Kiruthiga Udayakumar
January 13, 2026 AT 06:40My brother got this done last year. He’s a truck driver. Used to miss radio announcements, couldn’t hear horns behind him. Now? He says he hears brake squeals before he sees the car. He told me, ‘Sis, I don’t feel like I’m missing half the world anymore.’ That’s the real win. Not the tech. Not the cost. The peace.
Patty Walters
January 13, 2026 AT 20:45if you have chronic ear infections, DO THIS. i was told i’d never wear a hearing aid again. then i got the magnet one. no more gunk, no more pain, no more ‘sorry i can’t hear you’ every 5 mins. it’s not perfect but it’s the first thing in years that didn’t make me feel broken. also, the battery lasts forever. i forget to charge it for a week and it’s still good. 🙏
Jerian Lewis
January 14, 2026 AT 06:48Why do people treat this like a miracle? It’s a device. It doesn’t restore hearing. It redirects vibrations. You’re still hearing through a machine. And yes, you’ll still miss nuances. But I guess if you’re desperate enough, you’ll call it a gift.
Alicia Hasö
January 14, 2026 AT 23:54To anyone considering this: don’t wait. I was skeptical too. Thought it was sci-fi nonsense. But after 18 months of single-sided deafness, I was missing my daughter’s voice when she hugged me from behind. I cried during the first activation. Not because it was perfect-but because I finally felt whole again. You deserve to hear the world from all angles. This isn’t just a hearing aid. It’s a doorway back to connection.
Micheal Murdoch
January 15, 2026 AT 02:39It’s funny how we’re so quick to celebrate tech fixes but ignore the human cost. The surgeries, the cleaning, the MRI nightmares, the stigma of a metal post behind your ear. This isn’t just about sound-it’s about identity. Some people wear it like armor. Others hide it under their hair. The real innovation isn’t the device. It’s how people adapt, survive, and still find joy in the noise.
Ashley Kronenwetter
January 16, 2026 AT 19:54While bone conduction is clinically effective, it is imperative to note that candidacy requires a multidisciplinary evaluation including audiological, radiological, and surgical assessment. Not all patients are suitable, and expectations must be managed accordingly. This is not a consumer product.
Heather Wilson
January 18, 2026 AT 00:06Let’s not pretend this is a miracle. 23% MRI issues? 8% revision surgeries? That’s not innovation-that’s a liability. And who’s paying for the follow-ups? Insurance? You? Your kids? This is expensive band-aid medicine wrapped in tech bro hype. And don’t even get me started on the ‘invisible’ marketing. It’s not invisible-it’s just less obvious. You’re still a walking medical device.
tali murah
January 19, 2026 AT 10:42So you’re telling me a $7,000 device that requires surgery and still can’t handle MRI scans is the ‘best option’ for people with ear infections? And you call this progress? Meanwhile, in 2026, we have AI that can transcribe speech in real time and translate it to text on your phone. Maybe we should just… give people captions instead of drilling holes in their skulls?