Liver Cancer – What You Need to Know
If you’ve heard the term “liver cancer” and feel unsure where to start, you’re not alone. This page breaks down the basics so you can spot warning signs early and understand what doctors might recommend.
Common Symptoms
The liver can grow tumors without causing pain at first, which is why many people don’t notice anything until later. Typical clues include a persistent belly ache, especially in the upper right side, unexplained weight loss, and feeling unusually tired all the time.
You might also see swelling in your abdomen or legs, yellowing of the skin and eyes (jaundice), and dark urine. If you have any of these signs for more than a few weeks, it’s smart to talk to a health professional.
Risk Factors You Can Watch
Not everyone with liver cancer has a clear cause, but several habits raise the odds. Chronic hepatitis B or C infection is a major driver, as is heavy alcohol use that leads to cirrhosis. Being overweight, having diabetes, or eating a diet high in processed foods can also tip the balance.
People with a family history of liver disease should stay extra vigilant and get regular check‑ups. Vaccines for hepatitis B are widely available and cut risk dramatically.
Treatment Choices
When doctors confirm liver cancer, they look at tumor size, location, and overall liver function to pick a plan. Surgery can remove the tumor if it’s small and the liver is still healthy enough.
For larger or multiple tumors, ablation (using heat or cold to destroy cancer cells) often works well. Liver transplant is an option for some patients with advanced disease but limited spread.
Chemotherapy drugs given directly into the liver’s blood supply—called trans‑arterial chemoembolization (TACE)—help shrink tumors and slow growth. Newer targeted therapies, like sorafenib, block specific signals cancer cells need to survive.
Immunotherapy is also making headway, training the body’s own immune system to attack liver cancer. Your doctor will discuss side‑effects and how each option fits your lifestyle.
Living With Liver Cancer
Beyond medical treatment, everyday habits matter. Eating a balanced diet rich in fruits, vegetables, lean protein, and whole grains supports liver function. Cutting alcohol completely is essential, even if you’ve only had a drink now and then.
Staying active—walking, gentle cycling, or swimming—helps maintain weight and improves overall stamina. If fatigue is a problem, break tasks into smaller steps and rest when needed.
Emotional support can be just as important as physical care. Talking to friends, joining an online community, or seeing a counselor helps manage stress and anxiety.
What to Expect From Your Doctor Visits
During appointments you’ll likely get blood tests that check liver enzymes, imaging scans like ultrasound, CT or MRI, and possibly a biopsy to confirm the cancer type. Ask your doctor to explain each result in plain language; a good clinician will walk you through what the numbers mean.
Keep a notebook of symptoms, medication changes, and questions you want answered. This makes appointments more efficient and ensures nothing slips through the cracks.
Quick Checklist
- Watch for belly pain, jaundice, unexplained weight loss or fatigue.
- Know your risk factors: hepatitis, heavy alcohol use, obesity, diabetes.
- Get regular screenings if you have liver disease history.
- Discuss all treatment options—surgery, ablation, TACE, targeted drugs, immunotherapy.
- Adopt a liver‑friendly lifestyle: healthy diet, no alcohol, moderate exercise.
This guide gives you a solid starting point. If anything feels off, reach out to a health professional right away. Early detection and informed choices are the best weapons against liver cancer.
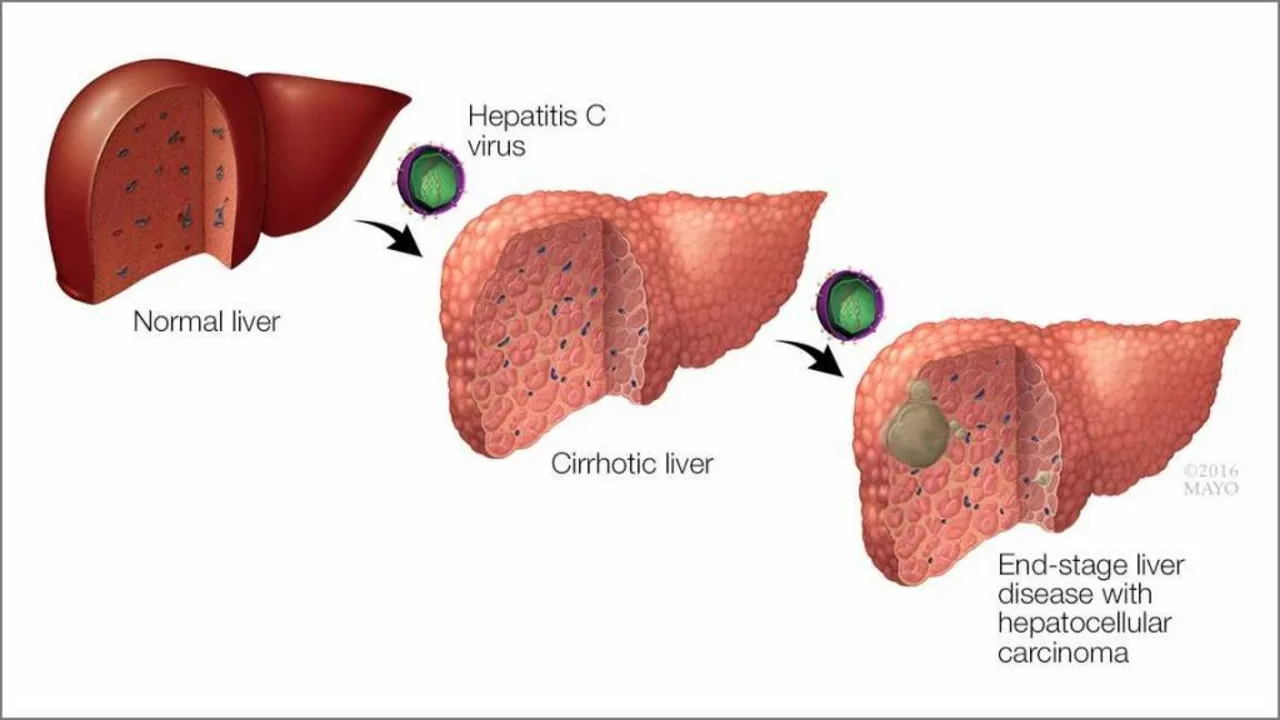
The Connection Between Genotype 3 Chronic Hepatitis C and Liver Cancer
In my recent exploration of medical research, I've discovered a significant connection between Genotype 3 Chronic Hepatitis C and liver cancer. Studies indicate that those with this specific genotype are at a higher risk of developing liver cancer. This risk is even greater for individuals with existing liver disease or damage. It's crucial for individuals with genotype 3 Chronic Hepatitis C to maintain regular medical check-ups to monitor liver health. Early detection and treatment can significantly reduce the chances of developing liver cancer.