When you pick up a prescription and see a different name on the bottle than what your doctor wrote, it’s natural to wonder: Is this really the same thing? The answer lies in a term you’ve probably never heard but use every time you save money on meds: pharmaceutical equivalence.
What Pharmaceutical Equivalence Actually Means
Pharmaceutical equivalence is the first rule in the game of generic drugs. It doesn’t mean the pill looks the same. It doesn’t mean the packaging matches. It doesn’t even mean the taste is identical. But it does mean this: the same active ingredient, in the same amount, in the same form, delivered the same way.
If your brand-name drug is a 10mg tablet of metoprolol taken by mouth, the generic version must contain exactly 10mg of metoprolol tartrate - no more, no less. It has to be a tablet. It has to be swallowed. The FDA requires this level of precision. The active ingredient - the part that actually treats your condition - must match down to the molecule.
This isn’t guesswork. Manufacturers test every batch using high-performance liquid chromatography (HPLC), a method that measures chemical composition with extreme accuracy. The active ingredient must fall within ±5% of the labeled amount. That’s stricter than many food products are held to.
And yes, the color, shape, and filler ingredients can be totally different. That’s why your generic lisinopril is blue and oval, while the brand is white and round. Those differences don’t matter - as long as the active ingredient is identical, the dosage form is the same, and the strength matches. That’s pharmaceutical equivalence in practice.
It’s Not the Whole Story - Bioequivalence Is What Comes Next
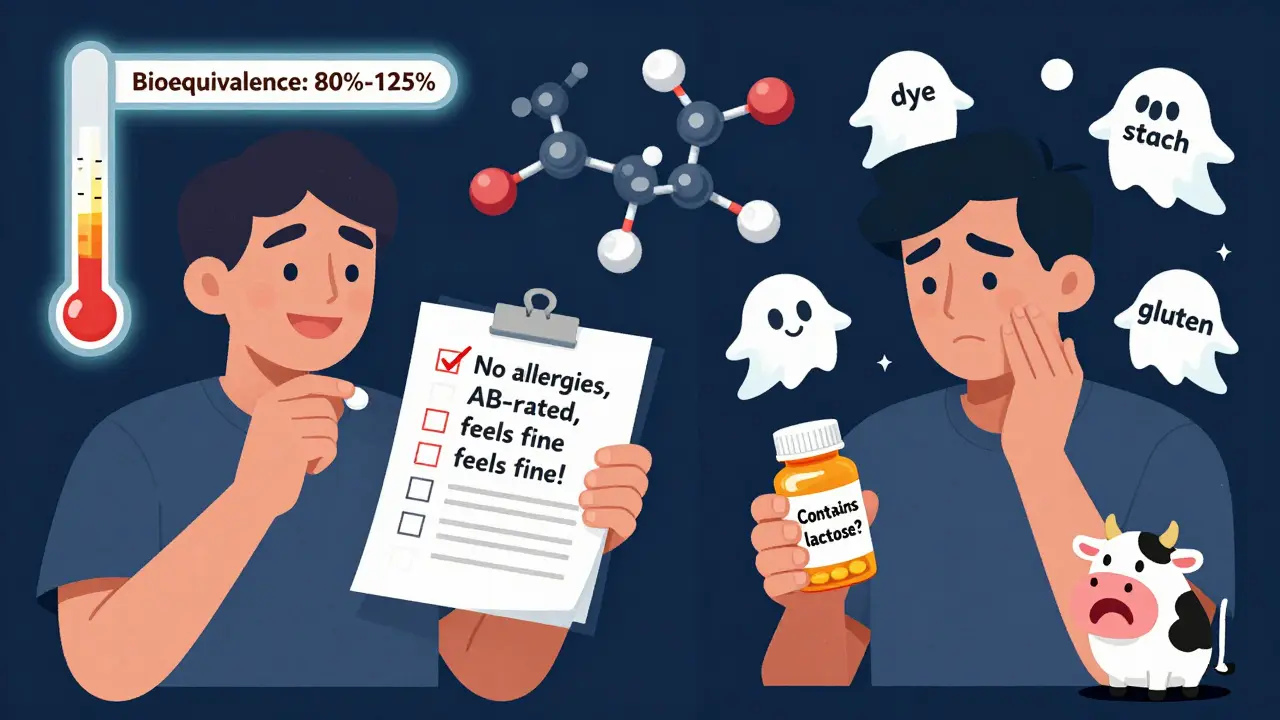
Here’s where people get confused. Just because two drugs are pharmaceutical equivalents doesn’t mean they’ll work exactly the same in your body. That’s where bioequivalence steps in.
Think of pharmaceutical equivalence as having the same engine. Bioequivalence is about whether that engine runs the same way on the road. A generic drug must deliver the active ingredient into your bloodstream at the same rate and to the same extent as the brand-name version. The FDA requires that the amount absorbed (measured as AUC) and the peak concentration (Cmax) fall between 80% and 125% of the brand-name drug. This range accounts for natural differences in how people absorb medications.
For most drugs, this works perfectly. But for drugs with a narrow therapeutic index - like warfarin, lithium, or levothyroxine - even small variations can matter. That’s why some generics for these drugs carry an “AB” rating in the FDA’s Orange Book (meaning they’re approved as interchangeable), while others are rated “BX” (meaning they’re not recommended for automatic substitution).
Pharmaceutical equivalence is the starting line. Bioequivalence is the race. You need both to be sure the generic will do the job without side effects or loss of effectiveness.
Why This Matters for Patients
Let’s say you’ve been on a brand-name statin for years. Your doctor switches you to the generic. You feel fine. No issues. That’s because pharmaceutical equivalence guarantees the same active ingredient. Bioequivalence ensures it gets absorbed the same way.
But sometimes, things go differently. A 2022 survey in the Journal of the American Pharmacists Association found that 87% of pharmacists had at least one patient report minor side effects after switching to a generic. Why? Not because the active ingredient changed - because of the fillers.
Generic drugs can use different inactive ingredients: dyes, preservatives, binders, or coatings. For most people, this is harmless. But if you’re allergic to lactose, or sensitive to food dyes like FD&C Red No. 40, or have celiac disease and the tablet contains gluten-containing starch - that’s when problems can arise. These aren’t covered under pharmaceutical equivalence. They’re hidden in the fine print.
That’s why pharmacists are trained to check your profile before substituting. If you’ve had a reaction before, they’ll flag it. And if you’re unsure, ask: “Is this generic safe for someone with a dairy allergy?” or “Does this contain gluten?” Most pharmacists will know.
How Pharmacists Use the Orange Book
The FDA’s “Approved Drug Products with Therapeutic Equivalence Evaluations” - better known as the Orange Book - is the bible for pharmacists. It lists every approved generic and rates it:
- AB: Therapeutically equivalent. Safe to substitute.
- BX: Not equivalent. Don’t swap.
- BZ: Insufficient data. Proceed with caution.
As of June 2024, over 12,800 generic drugs had an “AB” rating. That means they’ve passed both pharmaceutical and bioequivalence tests. These are the ones your pharmacist can switch you to automatically - and most do, unless you or your doctor say otherwise.
Hospitals follow strict policies. According to the American Society of Health-System Pharmacists, 68% require pharmacists to verify the Orange Book rating before switching a patient’s medication. That’s not bureaucracy - it’s safety.
Myths About Generic Drugs
There’s a myth floating around that generics contain only 80% of the active ingredient. That’s not true. That 80% number comes from the bioequivalence range - it’s the lower limit of absorption, not the amount of drug in the pill. The pill itself contains 100% of the labeled dose.
A 2023 Kaiser Family Foundation survey found 42% of patients believed generics were weaker. That misunderstanding costs people money and peace of mind. Generics aren’t “second-rate.” They’re scientifically identical in active ingredient, rigorously tested, and approved by the same agency that approves the brand names.
And they save money. From 2009 to 2023, generics saved the U.S. healthcare system over $2.2 trillion. On average, each generic prescription saves $1,008 compared to the brand-name version. That’s real savings - for patients, insurers, and taxpayers.
What’s Changing Now?
The FDA isn’t resting. In 2023, they launched the Complex Generic Drug Product Development Program to improve standards for harder-to-copy drugs - like inhalers, injectables, or topical creams. These aren’t as simple as swallowing a pill. The way the drug is delivered can affect how well it works.
Future rules may require more detailed testing of inactive ingredients, especially for patients with allergies. The FDA’s 2024 Strategic Plan includes $15 million for research into advanced techniques like Raman spectroscopy and X-ray diffraction to better analyze the physical structure of drugs. This isn’t about making generics harder to make - it’s about making sure even the most complex ones are truly equivalent.
Pharmacists are pushing for better labeling of inactive ingredients. Right now, you have to dig through the package insert. In the future, you might see a clear list on the bottle: “Contains lactose,” “No gluten,” “Contains FD&C Yellow No. 5.” That kind of transparency could prevent reactions and build trust.
What You Should Do
If you’re switching to a generic:
- Ask your pharmacist: “Is this rated AB in the Orange Book?”
- Check the label for inactive ingredients if you have allergies.
- Watch for changes in how you feel - especially with heart, thyroid, or seizure meds.
- Don’t assume all generics are the same. Two AB-rated versions of the same drug can still differ slightly in how they’re made.
- If something feels off after switching, talk to your doctor. It might be the filler, not the drug.
For most people, generics are safe, effective, and cheaper. Pharmaceutical equivalence makes that possible. But knowing the limits - and the details - helps you stay in control of your health.
Do generic drugs have the same active ingredient as brand-name drugs?
Yes. Pharmaceutical equivalence requires that generic drugs contain the exact same active pharmaceutical ingredient (API) as the brand-name drug, in the same amount and dosage form. The FDA mandates this through rigorous testing before approval. The only differences allowed are in inactive ingredients, color, shape, or packaging - none of which affect how the drug works in the body.
Are generic drugs as effective as brand-name drugs?
For most drugs, yes. If a generic is rated "AB" in the FDA’s Orange Book, it has passed both pharmaceutical equivalence (same active ingredient) and bioequivalence (same absorption into the bloodstream). This means it’s expected to work the same way clinically. However, for drugs with a narrow therapeutic index - like warfarin or levothyroxine - some patients may need to stay on the same brand or generic due to small differences in how their body processes the drug.
Why do some people have side effects after switching to a generic?
Side effects are usually caused by differences in inactive ingredients - like dyes, preservatives, or fillers - not the active drug. For example, someone with a lactose intolerance might react to a generic tablet that uses lactose as a binder, even if the brand-name version uses corn starch. These are rare, but real. If you notice new symptoms after switching, talk to your pharmacist or doctor. They can check the ingredients or switch you back.
Can I trust the FDA’s Orange Book ratings?
Yes. The Orange Book is updated monthly and is the official source for therapeutic equivalence ratings in the U.S. Drugs rated "AB" have been reviewed and approved by the FDA as interchangeable with the brand-name product. Pharmacists rely on this system to make substitutions safely. While rare exceptions exist - especially with complex drug delivery systems - the ratings are based on strict scientific standards and are widely trusted by healthcare providers.
How do I know if my generic is AB-rated?
Ask your pharmacist. Most pharmacies use electronic systems linked to the FDA’s Orange Book and will know the rating before filling your prescription. You can also check the FDA’s website directly by searching the drug name. If your generic is rated "AB," it’s considered interchangeable. If it’s rated "BX," your pharmacist should not substitute it without your doctor’s approval.





Erica Banatao Darilag
February 14, 2026 AT 21:29I’ve been on generics for years, and honestly, I’ve never had an issue. But I do read the label-especially since I’m lactose intolerant. I once got a generic that had lactose as a filler, and let me tell you, it wasn’t pretty. Now I always ask my pharmacist to check the inactive ingredients. It’s not that generics are bad-it’s just that we don’t talk enough about what’s *in* them, not just what they’re made of.
Kaye Alcaraz
February 16, 2026 AT 06:51Pharmaceutical equivalence is the foundation of safe, affordable healthcare. The FDA’s standards are not only rigorous but essential. What many fail to understand is that the active ingredient is not merely similar-it is identical. The science is precise. The regulatory framework is transparent. And the savings? Monumental. We must continue to champion this system-not because it’s convenient, but because it is scientifically sound and ethically imperative.
Sarah Barrett
February 17, 2026 AT 22:55It’s wild how much drama people make over pill color. I mean, if your meds are blue instead of white, you’re not getting a lesser version-you’re getting the same engine in a different paint job. The real villain? The mystery fillers. I had a cousin who broke out in hives after switching generics. Turned out it was a dye she’d never been exposed to before. We need labels that scream ‘Contains gluten’ or ‘Dairy alert’-not hide it in a 12-page insert like a treasure map to disaster.
Michael Page
February 18, 2026 AT 11:41The notion that equivalence implies interchangeability is a philosophical illusion. Even if two substances are chemically identical, the context of their delivery-the body, the environment, the individual’s microbiome-introduces irreducible variance. The FDA’s 80-125% bioequivalence window is not a scientific certainty but a statistical compromise. We mistake statistical tolerance for biological uniformity. This is not a flaw in generics-it is a flaw in our epistemological overconfidence.
Mandeep Singh
February 19, 2026 AT 00:31You people are so naive. The FDA? Please. They’re backed by Big Pharma. Generics are not ‘equivalent’-they’re cheaper knockoffs that cut corners. I worked in a lab in Mumbai. I’ve seen how these are made. The active ingredient? Maybe. But the binders? The coating? Sometimes they use industrial-grade starch. People get sick. People die. And you sit there saying ‘trust the Orange Book’ like it’s the Bible. It’s not. It’s a corporate loophole with a fancy name. If you’re on warfarin, you better stick with the brand-or you’re playing Russian roulette with your life.
Betty Kirby
February 20, 2026 AT 00:58Oh my god. Another one of these ‘trust the system’ rants. Let me guess-you’ve never had a generic make you feel like a zombie for three days? I did. Switched from brand to generic levothyroxine. Suddenly I was exhausted, gaining weight, forgetting my own phone number. My endocrinologist had to dig through the Orange Book and find the exact AB-rated version I’d been on. Turns out, not all AB-rated generics are created equal. The filler changed. My body noticed. And now I pay extra because I refuse to gamble with my thyroid. You want cheap? Fine. But don’t pretend it’s risk-free.
Josiah Demara
February 21, 2026 AT 23:18Let’s cut through the corporate fluff. The FDA’s Orange Book is a joke. ‘AB’ rating? That’s not a stamp of approval-it’s a license to profit. There are over 12,800 AB-rated generics? That means there are over 12,800 different companies making the same damn drug with different fillers, binders, and dyes. And somehow, we’re supposed to believe they’re all identical? I’ve seen batch-to-batch variations in HPLC data that would make a chemist weep. The system isn’t broken-it was designed this way. Generics aren’t cheaper because they’re better. They’re cheaper because they’re *less* controlled. And you’re all just too lazy to care.
Esha Pathak
February 23, 2026 AT 02:17Life is a journey, man. 🌿 I used to think generics were just ‘cheap drugs’-until I started studying Ayurveda and realized every medicine is a dance between element and intention. The active ingredient? Yes, same. But the energy? The vibration? Maybe not. I switched to a generic for my blood pressure and felt… off. Not sick. Just… disconnected. I went back to brand. And boom. Back to balance. Maybe science measures molecules. But healing? That’s deeper. Maybe we need to listen to our bodies-not just the Orange Book.
Mike Hammer
February 23, 2026 AT 10:35