When a doctor orders a brain MRI, it’s usually because something doesn’t add up. Maybe you’ve had unexplained headaches, trouble walking, memory lapses, or sudden weakness. Or perhaps you’re being monitored for a known condition like multiple sclerosis. The scan itself doesn’t tell you what’s wrong-it just shows you what’s there. And what it shows can be subtle, complex, and easy to misread if you don’t know what to look for.
What a Brain MRI Actually Shows
A brain MRI doesn’t use X-rays. Instead, it uses strong magnets and radio waves to map the water content and movement in your brain tissue. This gives it incredible detail-far more than a CT scan-especially in areas like the brainstem, cerebellum, and deep structures where bone can block other imaging methods.
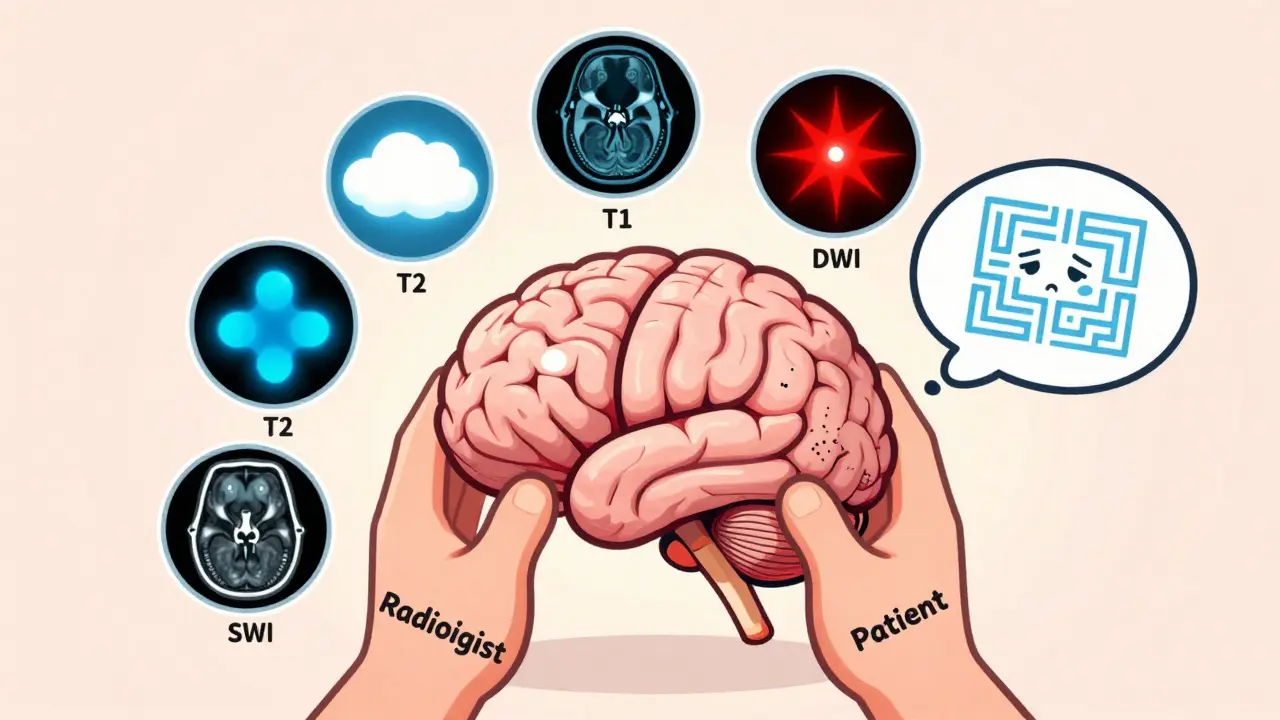
The real power of MRI comes from different scanning sequences. Each one highlights different tissue properties. Think of them like filters: one shows you fat, another shows you water, another shows you bleeding. You need all of them to get the full picture.
The Five Key MRI Sequences
- T1-weighted images are your anatomical roadmap. Fat looks bright white. Cerebrospinal fluid (CSF) is dark. Gray matter is slightly darker than white matter. This is where you check if the brain’s structure looks normal-size of ventricles, symmetry, position of brainstem.
- T2-weighted images are where pathology shines. Water = bright. That means swelling, tumors, infections, and old strokes all light up. But here’s the catch: CSF is also bright. So if you only look at T2, you might mistake a large ventricle for a lesion. That’s why you always compare it to FLAIR.
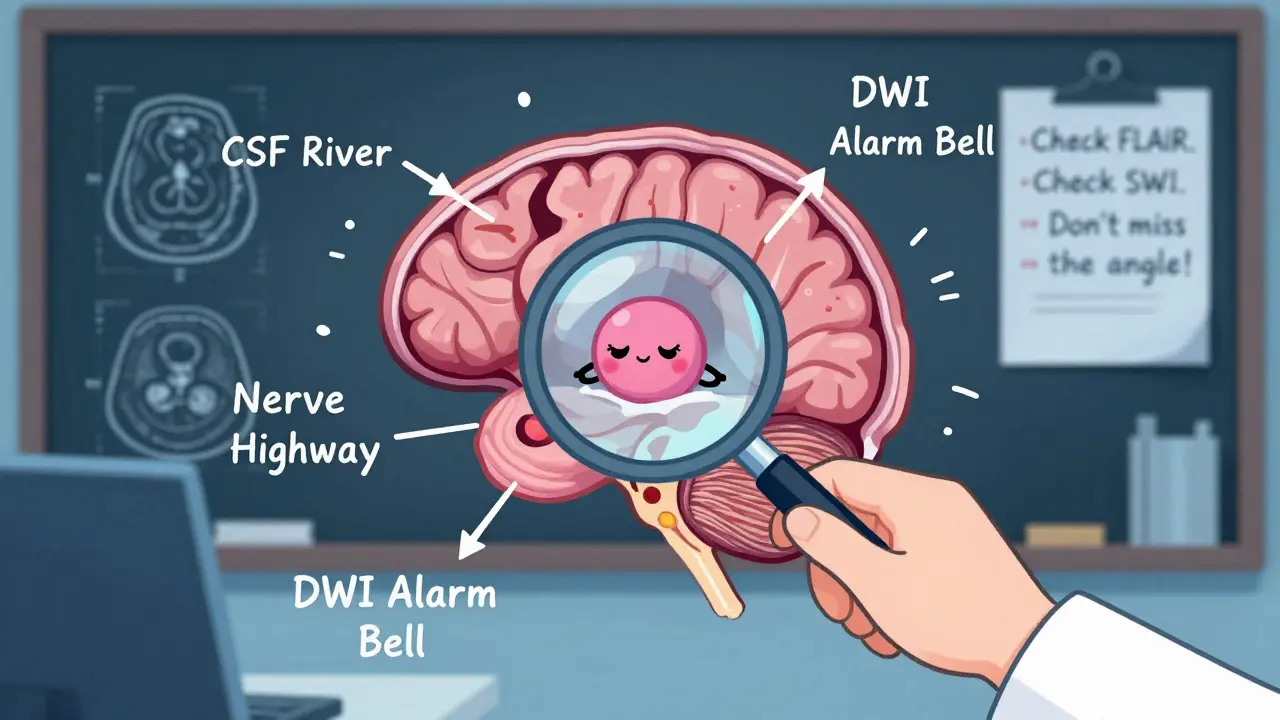
- FLAIR (Fluid-Attenuated Inversion Recovery) is the unsung hero. It turns CSF dark while keeping abnormal water (like from a stroke or MS plaque) bright. This is how radiologists spot lesions near the ventricles-exactly where multiple sclerosis likes to hide. If a bright spot disappears on FLAIR, it’s probably just CSF.
- Diffusion-weighted imaging (DWI) catches strokes within minutes. When brain cells die from lack of oxygen, water can’t move freely anymore. DWI picks that up as bright spots. The ADC map confirms it-if the spot is dark on ADC, it’s an acute stroke. If it’s bright, it’s just swelling. This difference changes whether someone gets clot-busting drugs or not.
- Susceptibility-weighted imaging (SWI) finds tiny bleeds. Even a few red blood cells stuck in the brain show up as dark specks. This is how you catch microhemorrhages from high blood pressure, amyloid angiopathy, or trauma. It’s also how you spot calcifications and iron deposits in Parkinson’s or Alzheimer’s.
Common Findings and What They Mean
Not every bright spot on an MRI is a disaster. Many are normal aging, others are silent, and some are red flags.
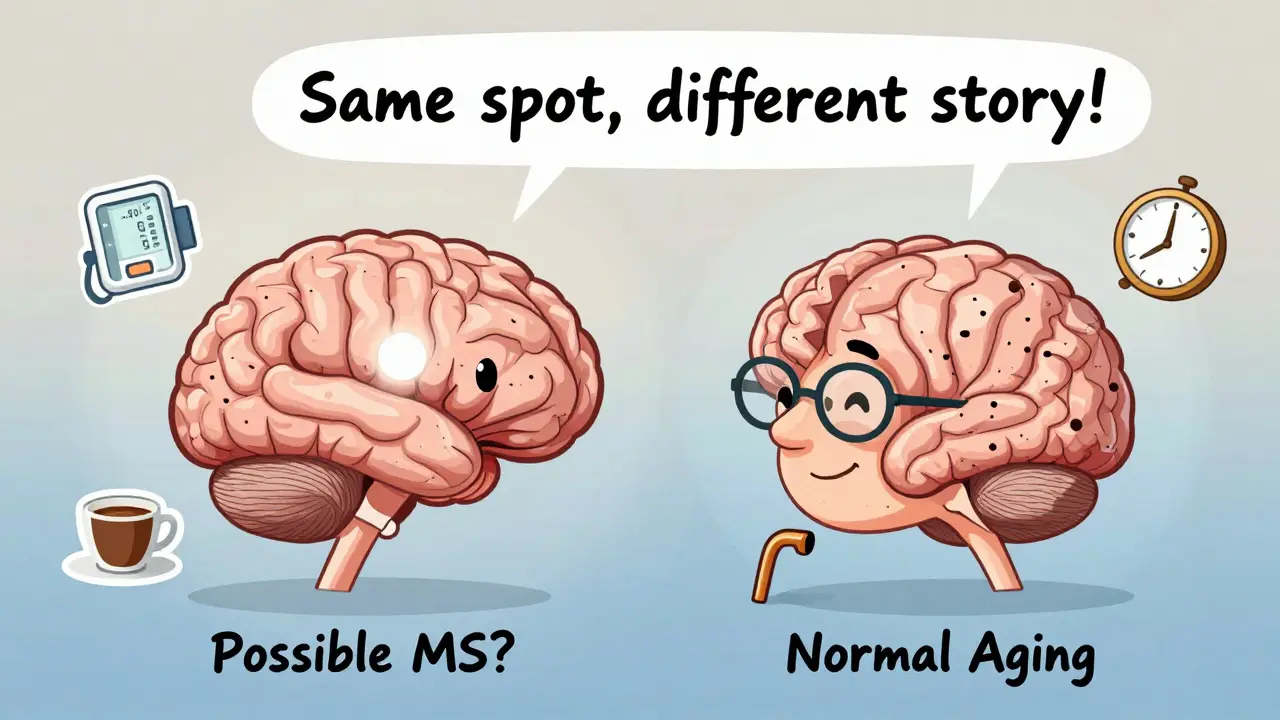
- White matter hyperintensities are small bright patches near the ventricles. They’re common in people over 60-even 90% of those over 70 have them. They’re linked to high blood pressure, diabetes, and aging. But if they’re large, asymmetric, or located in the corpus callosum, they might point to MS.
- Small lacunar infarcts are tiny strokes (3-5mm) in deep brain areas like the thalamus or basal ganglia. They often cause no symptoms. But if you find three or more, it suggests long-term uncontrolled hypertension. They’re a warning sign, not a crisis.
- Enlarged perivascular spaces (also called Virchow-Robin spaces) look like tiny black dots on T2 and FLAIR. They’re normal fluid-filled channels around blood vessels. But if they’re large or numerous, especially in the midbrain, they can mimic MS or other diseases. Location matters: they’re common in the basal ganglia and are usually harmless.
- Atrophy means brain shrinkage. Everyone loses some brain volume with age. But if the hippocampus (memory center) is significantly smaller than expected for your age, it raises suspicion for Alzheimer’s. If the whole brain is shrunken with wide ventricles, it might be vascular dementia or long-term alcohol use.
- Incidental tumors like vestibular schwannomas (acoustic neuromas) are often found by accident. They grow slowly on the hearing nerve. MRI can detect them as small as 2mm. If they’re under 1cm and not causing symptoms, they’re often just watched-no surgery needed.
What MRI Can’t Tell You
One big myth: MRI doesn’t show how someone feels. A person can have a massive lesion on their MRI and feel fine. Another person can have a normal scan and be in terrible pain.
Age matters. A 30-year-old with a small white matter lesion? It could be MS. A 75-year-old with the same lesion? Likely just aging. Location matters. A lesion in the temporal lobe could be herpes encephalitis. One in the parietal lobe? Maybe posterior reversible encephalopathy syndrome (PRES) from high blood pressure or preeclampsia.
And MRI can’t tell you when a lesion happened. A stroke from yesterday and one from five years ago can look identical on standard scans. That’s why doctors need your history. Did the weakness start suddenly? Was there a fall? Did you have a fever? The scan gives you anatomy. The story gives you context.
When MRI Isn’t the Right Choice
For a sudden, severe headache with vomiting and neck stiffness? A CT scan comes first-faster, better at spotting bleeding. For a head injury with loss of consciousness? CT wins. It takes 5 minutes. MRI takes 40.
And for routine migraines? The American College of Radiology says MRI is usually not appropriate. Only 1.3% of brain MRIs done for uncomplicated headaches show anything meaningful. That’s why guidelines warn against ordering them for “bad headaches” without neurological signs.
Also, MRI isn’t safe for everyone. Pacemakers, cochlear implants, and some metal fragments can be dangerous. Claustrophobia can ruin the scan. And if you’re in pain and can’t lie still, the images blur. That’s why CT still has a place-even in the age of advanced MRI.
How Radiologists Read a Brain MRI
There’s a method. It’s not guesswork.
Start in the middle: look at the ventricles. Are they enlarged? Is the septum pellucidum straight? Then move to the basal ganglia-check for small bright spots that could be old strokes. Then the cerebellum and brainstem-common spots for MS plaques and tumors. Then the cortex-look for swelling, thinning, or abnormal signals.
Always compare sequences. A bright spot on T2? Check FLAIR. If it’s still bright, it’s likely a lesion. If it disappears, it’s CSF. Is it dark on DWI? Then it’s not a stroke. Is it dark on SWI? Maybe a bleed.
And always check the cerebellopontine angle. That’s where acoustic neuromas hide. Miss it, and you miss a treatable tumor.
What’s New in Brain MRI
AI is cutting scan times in half. Software like Quantib can detect MS lesions automatically, reducing interpretation time from 20 minutes to 5. It’s not replacing radiologists-it’s helping them focus on the tricky cases.
Ultra-high-field 7T MRI is being used in research centers to see brain layers like never before. It’s not in hospitals yet, but it’s showing us how Alzheimer’s spreads through specific circuits.
Quantitative MRI is coming. Instead of just saying “there’s a lesion,” doctors will soon say “this lesion has a myelin water fraction of 18%,” which tells them if it’s active inflammation or old scar tissue. That’s huge for treatment decisions.
What You Should Know Before Your Scan
You don’t need to understand every sequence. But you should know this:
- Don’t panic if your report says “white matter changes.” It’s common. Ask: Is this normal for my age? Is it linked to my symptoms?
- Ask if contrast was used. It’s not always needed. But if a tumor or infection is suspected, contrast helps show where the blood-brain barrier is broken.
- If you’re being monitored for MS, ask about FLAIR and DWI. Those are the sequences that matter most.
- Don’t assume a normal MRI means nothing’s wrong. Some conditions-like early Parkinson’s or some types of epilepsy-don’t show up on standard scans.
Brain MRI is powerful, but it’s a tool-not a crystal ball. It shows structure, not function. It shows what’s there, not what’s causing your symptoms. That’s why your doctor’s questions, your history, and your physical exam still matter more than any image.
Can a brain MRI detect Alzheimer’s disease?
A standard brain MRI can’t diagnose Alzheimer’s directly, but it can show patterns consistent with it-especially shrinkage of the hippocampus and temporal lobes. In advanced cases, the brain may look significantly smaller than expected for age. However, a definitive diagnosis often requires PET scans that detect amyloid plaques. MRI is used more to rule out other causes like tumors, strokes, or normal pressure hydrocephalus that mimic Alzheimer’s symptoms.
Why do I need both T2 and FLAIR sequences?
T2 shows all water-rich areas, including cerebrospinal fluid (CSF), which also appears bright. FLAIR suppresses the CSF signal, making it dark, while keeping abnormal water (like from MS plaques or strokes) bright. This lets radiologists tell the difference between normal fluid spaces and actual brain lesions. Without FLAIR, you might mistake enlarged ventricles for disease.
Can an MRI show if a stroke is recent or old?
Yes, but only with the right sequences. Diffusion-weighted imaging (DWI) detects strokes within minutes to hours. If the lesion is bright on DWI and dark on ADC, it’s acute. If it’s dark on both, it’s likely old. Without DWI, it’s hard to tell. A lesion that looks bright on T2 or FLAIR could be days, weeks, or years old-those sequences don’t distinguish timing well.
Are brain MRI findings always meaningful?
No. Many findings are incidental and harmless. White matter hyperintensities are found in 90% of people over 70. Tiny cysts, enlarged perivascular spaces, and small old strokes often cause no symptoms. The key is matching findings to your symptoms. A radiologist may report “abnormalities,” but your doctor decides what matters for your health.
Why is MRI preferred over CT for neurological issues?
MRI provides up to 100 times better soft tissue contrast than CT, making it far better at detecting subtle changes like early MS plaques, small tumors, or inflammation. It also shows the posterior fossa (back of the brain) without bone interference, where CT often misses problems. Plus, MRI doesn’t use radiation, so it’s safer for repeated scans-important for conditions like epilepsy or MS that need long-term monitoring.



Sam Black
December 23, 2025 AT 00:06Man, I remember when I first saw my dad's MRI after his mini-stroke. All those bright spots on T2 had me convinced he was one bad scan away from a coma. Turns out? Most were just old lacunar infarcts. Funny how the brain keeps a record of every little bump and bruise. It's like your body's autobiography written in water.
Cara Hritz
December 24, 2025 AT 07:31wait so FLAIR makes CSF dark but lesions stay bright?? i always thought the bright stuff was bad but now i get it lol
Kathryn Weymouth
December 25, 2025 AT 09:12It's fascinating how much we've learned about brain anatomy through these sequences. T1 gives us structure, T2 reveals pathology, FLAIR filters out the noise, DWI catches strokes in real time, and SWI picks up the tiniest hemorrhages. Each sequence is like a different lens on reality-without one, the picture is incomplete. And yet, we still rely on the patient’s story to make sense of it all. The machine sees tissue; the human sees meaning.
Art Van Gelder
December 26, 2025 AT 06:30Let me tell you, I once had a neurologist look at my MRI and say, 'Oh, these white matter changes are just aging.' I was 42. I spent three weeks Googling until I was convinced I had early-onset MS. Turns out? I was just stressed, sleep-deprived, and had high blood pressure from drinking too much coffee. The scan didn’t lie-but it didn’t tell the whole truth either. That’s the thing about MRI: it shows you what’s there, but not why you’re here.
Jamison Kissh
December 28, 2025 AT 03:42If a brain is a library, then MRI is the catalog. It lists every book, every shelf, every faded spine. But it doesn’t tell you who read them, when, or why. A lesion isn’t a diagnosis-it’s a footnote. And the real story? That’s written in the patient’s voice, their pain, their memories, their fear. We’ve outsourced understanding to machines, but the soul of medicine still lives in the conversation.
Tarun Sharma
December 28, 2025 AT 14:33Thank you for this clear explanation. I work in healthcare and appreciate accurate technical information presented without sensationalism.
Julie Chavassieux
December 30, 2025 AT 13:44So... if my MRI shows 'incidental findings'... does that mean I'm secretly dying? Or just... mildly broken? 🤔
Aliyu Sani
December 31, 2025 AT 04:33bro the SWI sequence is wild-like your brain’s got tiny blood ghosts everywhere. I had a friend with hypertension and his scan looked like a starfield of microbleeds. Scary shit. But doc said if he controls BP, they ain’t gonna kill him tomorrow. Just a slow leak.
Tony Du bled
January 1, 2026 AT 21:37Just got my results back. 'Mild white matter hyperintensities.' I asked the doc if I should panic. He said, 'Do you feel like you're losing your mind?' I said no. He said then don't worry about it. I left feeling like I'd been given a free pass to keep being a normal weirdo.
Candy Cotton
January 2, 2026 AT 02:07It is imperative to underscore that the utilization of magnetic resonance imaging in the context of neurological diagnostics constitutes a paradigmatic advancement in clinical medicine. The differential sequence analysis, particularly the strategic employment of FLAIR and DWI modalities, permits the radiologist to discern pathologic entities with unprecedented precision. One must not conflate incidental radiographic findings with clinical pathology. The American College of Radiology guidelines are unequivocal: routine imaging for uncomplicated headaches is not evidence-based. This is not conjecture; it is science.
Jim Brown
January 4, 2026 AT 01:18There’s something poetic about how we’ve built machines that can see the invisible-water trapped in dying cells, blood the size of a grain of salt, the slow erosion of memory centers. But we still can’t measure loneliness, or grief, or the quiet terror of waiting for a diagnosis. Maybe the real breakthrough isn’t in the magnets or the algorithms, but in remembering that the most important sequence is the one between doctor and patient-the one where someone says, ‘I see you.’