What Is Allergic Asthma, Really?
Allergic asthma isn't just asthma that gets worse when you sneeze. It's a specific type where your immune system mistakes harmless stuff like pollen, dust mites, or cat dander for invaders. When you breathe them in, your body releases IgE antibodies, which trigger mast cells to dump histamine and other inflammatory chemicals into your airways. That’s what causes the tightening, swelling, and mucus buildup - the classic asthma symptoms: wheezing, coughing, chest tightness, and shortness of breath.
This isn't rare. About 60% of the 25 million Americans with asthma have this form, according to the American College of Allergy, Asthma, and Immunology. In kids, it’s even higher - over 80% of pediatric asthma cases are allergic. The big difference between allergic and non-allergic asthma? You can often find and avoid the triggers. That’s the key to taking control.
What’s Actually Triggering Your Asthma?
Not all allergens are created equal, and they don’t all show up at the same time. Knowing which ones are hitting you can make all the difference.
- Tree pollen: Hits hard from February to April, especially in March. In many areas, counts hit 10-20 grains per cubic meter. If you’re sensitive, even low counts can spark symptoms.
- Grass pollen: The June culprit. Counts can jump to 50-100 grains per cubic meter. Lawn mowing? That’s basically an asthma attack waiting to happen.
- Ragweed pollen: Peaks in September. It’s the most potent outdoor allergen in the U.S. - counts often exceed 100 grains per cubic meter. Thunderstorms during ragweed season can cause emergency room spikes because wind breaks up pollen grains into even smaller, inhalable pieces.
- Dust mites: These aren’t bugs you can see. They live in bedding, carpets, and upholstered furniture. The allergen? Their poop. And they thrive where humidity is above 50%. In 84% of U.S. homes, levels are high enough to trigger sensitization - that’s more than 3 out of 4 households.
- Cat dander: The protein Fel d 1 clings to fur, skin, and even clothes. It’s so sticky, it stays airborne for hours. You don’t even need a cat in the house - 79% of U.S. homes have enough Fel d 1 to cause problems, even if no cat lives there.
- Mold: Alternaria spores explode during late summer storms. When counts go above 500 spores per cubic meter, ER visits for asthma jump 3.5 times. Basements, bathrooms, and leaky roofs are prime breeding zones.
Some triggers are seasonal. Others? They’re in your bedroom right now.
How to Actually Avoid Allergens (Not Just the Basics)
"Just clean your house" isn’t enough. You need targeted, measurable steps.
- Bedding: Use allergen-proof covers (not just "hypoallergenic") on your mattress, box spring, and pillows. Look for a pore size under 10 microns - that’s what blocks dust mites. Replace old bedding if it’s more than 5 years old. Wash everything weekly in water hotter than 130°F. Cold water? Doesn’t kill mites or remove allergens.
- Vacuuming: Use a vacuum with a true HEPA filter. Regular vacuums just blow dust back into the air. Vacuum at least twice a week. If you can’t, get someone else to do it - or wear an N95 mask while you do.
- Humidity control: Keep indoor humidity between 30% and 50%. Use a hygrometer to check. If it’s above 50%, dust mites multiply. Below 30%, your airways dry out and get more sensitive. A whole-house dehumidifier like the AprilAire 500M can cut dust mite allergens from 20 µg/g to under 0.5 µg/g.
- Cats and dogs: If you’re allergic to cats, keeping the cat out of the bedroom isn’t enough. Bathe your cat weekly - it reduces Fel d 1 by up to 80%. Use a HEPA air purifier in the bedroom. If you can’t tolerate the allergen levels, rehoming may be the most effective long-term solution.
- Pollen: Check daily pollen counts (National Allergy Bureau app is reliable). Keep windows closed when counts exceed 9.7 grains/m³. Shower and change clothes after being outside. Don’t hang laundry outside - pollen sticks to fabric. Wear an N95 mask during yard work - it cuts exposure by 85%.
- Indoor air quality: Avoid smoking indoors. PM2.5 pollution (from fireplaces, candles, or traffic) makes your airway lining more permeable, letting allergens slip in easier. Air purifiers with HEPA and activated carbon filters help - but only if they’re sized for the room.
One Reddit user with severe dust mite asthma reported their peak flow jumped from 380 to 470 L/min after implementing all these steps over six months. That’s not luck - that’s science.

Immunotherapy: The Only Treatment That Changes the Disease
Medications like inhalers and antihistamines treat symptoms. Immunotherapy treats the cause.
There are two main types:
- Subcutaneous Immunotherapy (SCIT): Allergy shots. You get weekly injections for 4-6 months, building up to a maintenance dose. Then you go monthly for 3-5 years. It’s the gold standard. Studies show it reduces asthma symptoms by 30-50% more than medication alone. The 2021 Cochrane review of over 12,000 people found it cuts the need for asthma meds by up to 40%.
- Sublingual Immunotherapy (SLIT): Daily tablets or drops under the tongue. Less invasive. No needles. But you have to take it every single day. It’s approved for grass, ragweed, and dust mites. The MILO trial showed SLIT cut dust mite asthma symptoms by 35% - compared to just 15% with inhaled steroids alone.
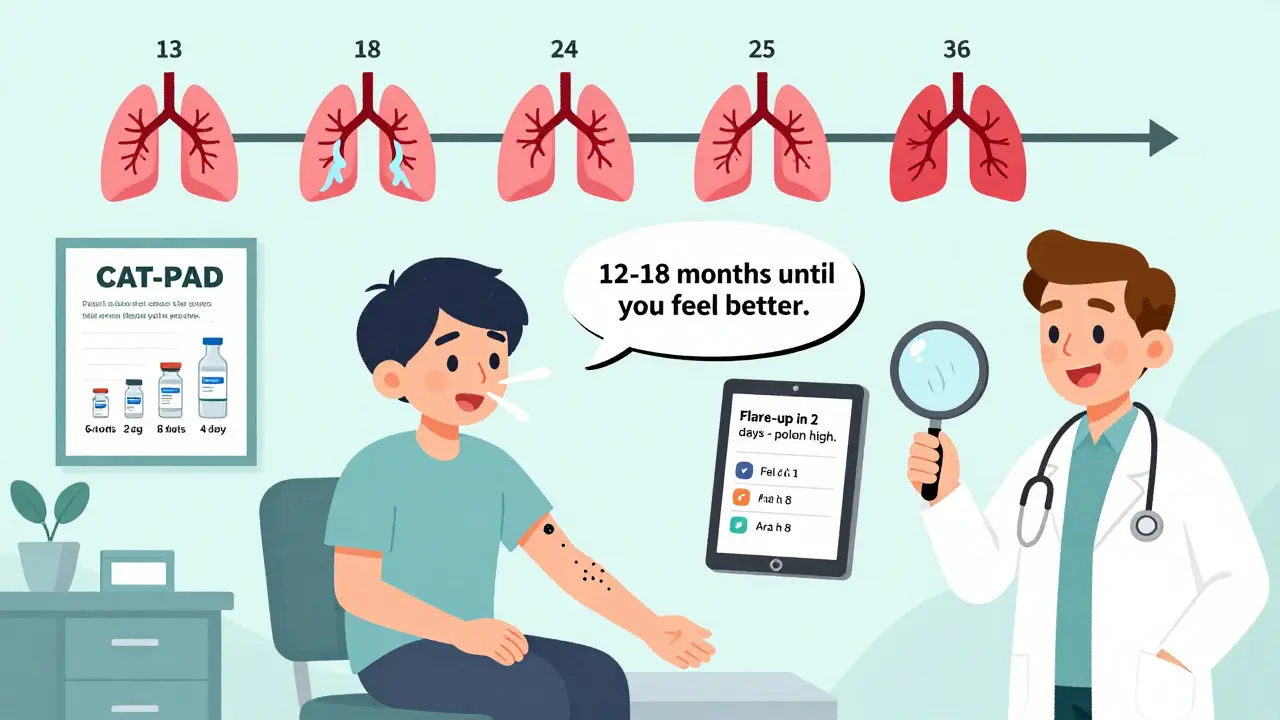
It’s not instant. Most people start feeling better after 12-18 months. Full benefit takes 3-5 years. But the payoff? Long-term remission. The PAT study showed patients who completed 3-5 years of immunotherapy still had fewer symptoms 10 years later.
Side effects? SCIT can cause local swelling or, rarely, anaphylaxis - that’s why shots are given in a doctor’s office. SLIT often causes mild mouth itching at first - 78% of users report it in the first month. Most stop noticing after a few weeks.
Who Shouldn’t Try Immunotherapy?
It’s not for everyone. If you have unstable asthma (recent ER visits or steroid bursts), immunotherapy can be risky. You need to be on stable meds first.
Also, not all allergic asthma is the same. About 30% of people diagnosed with allergic asthma don’t actually have the type 2 inflammation that responds to IgE-targeting treatments. That’s why doctors now check blood eosinophils and FeNO (fractional exhaled nitric oxide) levels. If your eosinophils are below 300 cells/µL and FeNO is under 25 ppb, immunotherapy might not help - even if your skin test is positive.
And cost? SCIT costs about $18.90 per shot with Medicare. SLIT tablets cost $500-$1,000 per month without insurance. But over time, you’ll likely spend less than you do on inhalers, nebulizers, and emergency visits.
The Future: Precision Asthma Care
Things are changing fast. The NIH is testing genetic markers to predict who will respond to immunotherapy - with 85% accuracy. New tools like the Allergen Insight nasal sensor can detect airborne allergens at 0.1 µg/m³ and send alerts to your phone. AI platforms like AsthmaIQ combine pollen forecasts, your medication logs, and even your sleep data to predict flare-ups 2-3 days ahead - with 92% sensitivity.
There’s also new immunotherapy on the horizon. CAT-PAD, a peptide-based cat dander treatment, cuts the build-up phase from 6 months to just 8 weeks. A pollen vaccine (Pollen-VLP) showed 60% symptom reduction with only 4 doses a year in Phase III trials.
By 2030, doctors may use molecular allergen testing - not just "pollen," but specific proteins like Ara h 8 (linked to birch-pollen food syndrome) or Alternaria alternata IgE levels - to tailor treatment. That means fewer people wasting time and money on treatments that won’t work for them.
Real Talk: What Works, What Doesn’t
People on Reddit say things like, "I bought an air purifier and nothing changed." Why? Because they didn’t fix the bed, didn’t control humidity, and kept the cat in the bedroom. You can’t out-filter a house that’s full of allergens.
Others say, "I did shots for a year and felt worse." That’s because they stopped too soon. Immunotherapy isn’t a quick fix. It’s a long-term investment in your immune system.
The most successful patients? They track their symptoms. They know their triggers. They don’t just rely on inhalers. They combine avoidance with immunotherapy when needed. And they stick with it.
What to Do Next
If you think you have allergic asthma:
- Get tested. Skin prick or blood IgE test to find your triggers.
- Measure your environment. Buy a hygrometer. Check your home for dust mites and mold.
- Start with avoidance. Change bedding, control humidity, vacuum with HEPA.
- See an allergist. If symptoms persist despite avoidance, talk about immunotherapy.
- Track your progress. Use a peak flow meter. Note when symptoms worsen.
You don’t have to live with daily wheezing. Allergic asthma is manageable - if you know what’s causing it and how to fight back.
Can you outgrow allergic asthma?
Some children do, especially if their triggers are controlled early. But for adults, allergic asthma usually doesn’t go away on its own. Immunotherapy can induce long-term remission - meaning symptoms disappear for years, even after stopping treatment. The PAT study showed 60% of patients remained symptom-free 10 years after completing 3-5 years of immunotherapy.
Are allergy shots worth the pain and cost?
For people with confirmed allergic asthma who don’t respond well to meds, yes. They reduce the need for inhalers and prevent emergency visits. Over 5 years, most patients save more on medications and missed work than they spend on shots. Medicare and many insurers cover 80% of the cost. The real cost is not doing it - ongoing symptoms, lost sleep, and higher long-term healthcare use.
Can you do immunotherapy for multiple allergens at once?
Yes. Most allergy shots include 3-6 allergens - like dust mites, grass, and ragweed - mixed in one vial. SLIT tablets are single-allergen, but you can take multiple tablets daily. Your allergist will test you to find which allergens are actually causing your symptoms. There’s no benefit to treating something you’re not truly allergic to.
Do air purifiers really help with asthma?
Only if they have a true HEPA filter and are the right size for the room. They help reduce airborne allergens like pollen and pet dander. But they don’t remove dust mites from bedding or mold from walls. They’re a tool - not a cure. Best used with other avoidance steps, like washing bedding and controlling humidity.
Is allergic asthma worse than non-allergic asthma?
Not necessarily worse - but different. Allergic asthma often starts younger and responds better to targeted treatments like biologics and immunotherapy. Non-allergic asthma is harder to predict and avoid triggers for, but responds better to things like bronchial thermoplasty or macrolide antibiotics. The key is identifying which type you have so you get the right treatment.





Sazzy De
January 31, 2026 AT 10:12Beth Beltway
February 1, 2026 AT 10:38Jason Xin
February 2, 2026 AT 23:06Holly Robin
February 3, 2026 AT 06:19April Allen
February 4, 2026 AT 11:36Amy Insalaco
February 4, 2026 AT 14:58Bobbi Van Riet
February 5, 2026 AT 02:17Kathleen Riley
February 6, 2026 AT 00:58Gaurav Meena
February 8, 2026 AT 00:47Katie and Nathan Milburn
February 9, 2026 AT 16:42Marc Bains
February 11, 2026 AT 11:55Sarah Blevins
February 13, 2026 AT 04:56Yanaton Whittaker
February 14, 2026 AT 16:47Jodi Olson
February 16, 2026 AT 14:07